Weighing the Advantages and Disadvantages of Insulin Pump Therapy

Why Understanding Insulin Pump Therapy Matters for Better Diabetes Control
The advantages and disadvantages of insulin pump therapy represent one of the most important decisions you'll make in managing your diabetes. With over 350,000 Americans now using insulin pumps - a dramatic increase from fewer than 7,000 users in 1990 - this technology has become a cornerstone of modern diabetes care.
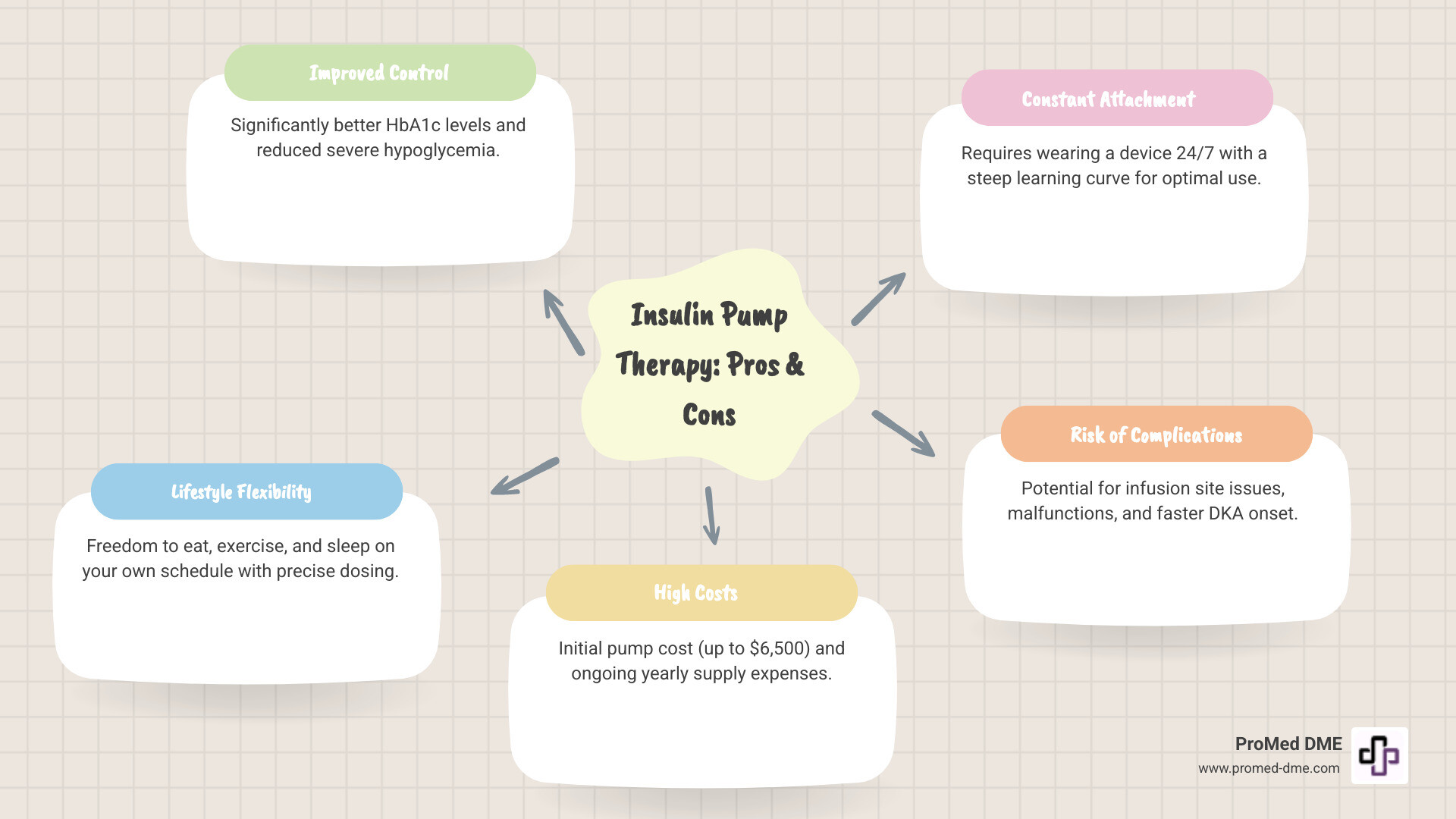
Key Advantages:
- Better blood sugar control - Studies show improved HbA1c levels in 20 out of 23 pediatric studies
- Fewer severe low blood sugar episodes - 80% of adult studies showed reduced hypoglycemia
- Lifestyle flexibility - Eat, exercise, and sleep on your schedule
- Precise dosing - Deliver insulin in increments as small as 0.025 units
- Fewer injections - Change infusion set every 2-3 days instead of daily shots
Key Disadvantages:
- High cost - Pumps cost up to $6,500, plus $2,000-$3,000 yearly for supplies
- Constant attachment - Wear the device 24/7
- Learning curve - Requires extensive training and commitment
- Risk of complications - Skin infections, pump malfunctions, faster onset of diabetic ketoacidosis
- Frequent monitoring - Need to check blood sugar at least 4-6 times daily
For many, an insulin pump can provide a feeling of being more in control of their diabetes and their life. However, it's not the right choice for everyone. The decision requires careful consideration of your lifestyle, health goals, and personal preferences.
Advantages and disadvantages of insulin pump therapy further reading:
- aace guidelines for insulin pump therapy
- continuous glucose monitoring system
- how to use insulin pump therapy
What Is an Insulin Pump and How Does It Work?
An insulin pump, also known as Continuous Subcutaneous Insulin Infusion (CSII), is a small, smart device that delivers insulin continuously to help manage your blood sugar levels around the clock. Unlike multiple daily injections (MDI), a pump provides a steady, precise flow of insulin, aiming to mimic the natural release from a healthy pancreas.
An insulin pump system has a few key components:
- The pump body: This small electronic device, about the size of a small mobile phone, is the control center. Some models are even smaller, and tubeless "patch pumps" attach directly to the skin for discretion.
- An insulin reservoir or cartridge: This container holds the rapid-acting insulin used in the pump. Pumps do not use long-acting insulin.
- An infusion set: This connects the pump to your body. For tubed pumps, it consists of a thin plastic tube (catheter) and a small cannula inserted under the skin. Patch pumps have an integrated cannula.

So, how does this system work?
Basal Rate Delivery: The pump delivers a continuous, small amount of insulin 24/7, known as your "basal rate." This background insulin keeps blood sugar stable between meals and overnight. Pumps offer incredible precision, delivering basal rates in increments as small as 0.01 units per hour. This helps manage issues like the "dawn phenomenon" (an early morning rise in blood sugar) and is beneficial for those needing small doses, like children or athletes. More info about basal insulin
Bolus Doses for Meals and Corrections: When you eat or need to correct high blood sugar, you direct the pump to deliver a larger, on-demand dose called a "bolus." Most pumps include a "bolus wizard" or built-in calculator to help determine the correct dose based on your blood glucose and carb intake. Bolus doses can also be delivered with high precision (as small as 0.025 units), allowing for accurate insulin matching to food.
The key to understanding the advantages and disadvantages of insulin pump therapy is its customization. You can program different basal rates for different times of day and deliver flexible bolus doses as needed. This personalization allows the pump to mimic the body's natural insulin release, often leading to better blood sugar control and a more flexible lifestyle.
A Deep Dive into the Advantages and Disadvantages of Insulin Pump Therapy
Deciding on insulin pump therapy is a significant step. It offers many benefits that can profoundly impact daily life, but it also comes with challenges and commitments. Let's explore the comprehensive advantages and disadvantages of insulin pump therapy.
The Advantages: Gaining Tighter Control and Lifestyle Flexibility
Insulin pump therapy has revolutionized diabetes management for many, offering a level of control and flexibility that traditional injections often cannot match.
- Improved HbA1c Levels: A major advantage is the potential for better glycemic control. Studies consistently show that pump therapy can lead to significant improvements in HbA1c (a three-month average of blood sugar). A lower HbA1c is directly linked to a reduced risk of long-term diabetes complications.
- Reduced Severe Hypoglycemia: The precise, continuous insulin delivery and advanced pump features significantly reduce the incidence of severe hypoglycemia (dangerously low blood sugar). Research shows a dramatic drop in these events for both adults and children using pumps, which is a huge relief for many.
- Fewer Daily Injections: Pump therapy drastically reduces needle sticks. Instead of multiple daily injections, you only change your infusion set (which includes inserting a new cannula) every 2 to 3 days. Many find this far less burdensome than frequent injections.
- Mealtime Flexibility: Pumps offer unparalleled freedom around food. You can easily deliver an insulin bolus for a spontaneous meal or snack without an extra shot. The pump’s bolus wizard helps calculate the right amount, allowing for less rigid meal scheduling. You can also use extended boluses for high-fat meals to prevent delayed blood sugar spikes.
- Precise Dosing Increments: Pumps deliver insulin in tiny increments – as little as 0.01 unit/hour for basal rates and 0.025 units for bolus doses. This micro-dosing is especially beneficial for insulin-sensitive individuals, like young children or active adults.
- Customizable Basal Rates: Your body's insulin needs change throughout the day. Pumps allow you to program different basal rates for different times, which is a game-changer for managing the "dawn phenomenon" (a morning blood sugar rise) or adjusting for illness.
- Easier Exercise Management: Exercise can make blood sugar unpredictable, but pumps help manage it. You can temporarily lower your basal rate to prevent low blood sugar during and after physical activity, offering greater freedom to stay active.
- Better Control of Dawn Phenomenon: Affecting over half of people with diabetes, this natural early morning rise in blood sugar can be countered by programming the pump to deliver a higher basal rate during these hours, leading to more stable morning glucose levels.
- Reduced Risk of Long-Term Complications: The combination of improved blood glucose control, lower HbA1c, and fewer severe hypoglycemic episodes contributes to a lower risk of developing long-term diabetes complications.
The National Institute for Health and Care Excellence (NICE) has reviewed extensive research supporting these benefits. NICE research on pump benefits
The Disadvantages: Cost, Complications, and Constant Commitment
While the advantages are compelling, it's crucial to consider the other side of the coin.
- High Initial and Ongoing Costs: This is a major hurdle. A pump can cost up to $6,500, with supplies like infusion sets and reservoirs adding another $2,000-$3,000 annually. While many insurance plans, like those we work with at ProMed DME, offer coverage, out-of-pocket expenses can still be substantial.
- Insurance Navigation: Securing insurance coverage for a pump and its supplies can be a complex and time-consuming process. Navigating approvals and understanding benefits requires patience and persistence.
- 24/7 Device Attachment: This is a common psychological and practical challenge. Being attached to a device 24/7 can cause body image concerns for some, and the tubing can occasionally get caught on things. Managing the pump during intimacy, showering, or sports requires planning.
- Risk of Infusion Site Failure: If your infusion set fails (e.g., a bent cannula or air bubble), insulin delivery can be interrupted. This can lead to high blood sugar levels quickly, so you must be diligent about checking your site and pump.
- Skin Irritation and Infections: The infusion site can sometimes develop irritation, allergic reactions to adhesives, or infections. Proper site rotation and good hygiene are crucial to minimize these risks, though serious infections are rare.
- Potential for Pump Malfunction: Like any electronic device, pumps can fail. Though rare, a malfunction means no insulin delivery. It's essential to always have a backup plan and supplies (like a vial and syringe).
- Steep Learning Curve: Pump therapy is not a "set it and forget it" solution. It requires extensive training to learn how to program the pump, calculate doses, and troubleshoot problems. It also demands a commitment to frequent blood glucose monitoring and accurate carbohydrate counting.
- Increased Risk of Diabetic Ketoacidosis (DKA): Because pumps use only rapid-acting insulin, an interruption in delivery can lead to DKA more quickly than with long-acting injections. However, studies suggest that with proper training and vigilance, this risk can be effectively managed.
The Evolution of Pumps: Sensor-Augmented and Automated Systems
Insulin pump technology has advanced significantly, moving far beyond simple mechanical devices. Today's advantages and disadvantages of insulin pump therapy include cutting-edge systems that are bringing us closer to an artificial pancreas.

This evolution began with Continuous Glucose Monitors (CGMs), which measure glucose levels in the fluid under the skin, providing real-time readings every few minutes. This gives a continuous view of glucose trends, rather than single snapshots from finger pricks.
The next step was combining CGMs with pumps to create Sensor-Augmented Pumps (SAP). These systems display glucose data on the pump screen, helping users make better dosing decisions. Studies show SAP systems lead to a greater reduction in A1C levels (about 0.8% improvement) after 12 months compared to injection therapy.
Further innovation led to pumps that automatically respond to glucose readings, such as those with hypoglycemia suspension features.
Low Glucose Suspend (LGS) systems automatically pause insulin delivery when glucose drops below a preset threshold, reducing hypoglycemia episodes by 40-50%.
More advanced Predictive Low Glucose Suspend (PLGS) technology uses algorithms to predict and prevent lows before they happen. PLGS can reduce overnight hypoglycemia by 50-80% and overall hypoglycemia by 31-50% compared to basic SAP systems.
The most advanced technology available is the Hybrid Closed-Loop (HCL) system, also known as automated insulin delivery. These systems combine a CGM, an insulin pump, and an advanced algorithm. The algorithm uses real-time glucose data to automatically adjust background insulin delivery to keep blood sugar in a target range. While users still need to bolus for meals, these systems dramatically reduce the daily burden of diabetes management.
Studies show Hybrid Closed-Loop systems decrease A1C levels by about 0.5% and increase time-in-range by approximately 8% after three months. These advances offer greater precision, safety, and peace of mind.
For those interested in the clinical research, A clinical overview of modern insulin pump therapy provides comprehensive insights into how these systems are revolutionizing diabetes care.
Is Insulin Pump Therapy the Right Choice for You?
Choosing to start insulin pump therapy is a personal decision. How the advantages and disadvantages of insulin pump therapy fit into your life is what matters most. An open conversation with your healthcare team is essential to determine if it's the right fit.
Profile of an Ideal Candidate for Insulin Pump Therapy
For many, an insulin pump can be a transformative tool for managing diabetes.
It's a common choice for individuals with Type 1 diabetes and can also benefit people with insulin-dependent Type 2 diabetes who struggle with multiple daily injections. Studies show Type 2 users can lower their A1C by 1.0% or more with pump therapy.
An ideal candidate is often:
- Motivated to improve control: Someone who is proactive and wants to fine-tune their diabetes management.
- Comfortable with technology: Users should be willing to learn and interact with a medical device and its settings.
- Experiencing frequent low blood sugar: Pumps, especially modern systems with suspension features, can significantly reduce hypoglycemia and provide peace of mind for those with hypoglycemia unawareness.
- Seeking lifestyle flexibility: A pump is ideal for those with unpredictable schedules, as it allows for on-the-fly adjustments for meals and exercise.
- Finding injections difficult: For those who find multiple daily injections cumbersome or painful, a pump offers a less intrusive alternative.
Pumps are also often recommended for specific clinical needs, such as gastroparesis (requiring extended boluses), pregnancy (where tight control is crucial), managing the dawn phenomenon, or for those who need very small insulin doses, like young children.
When Might an Insulin Pump Not Be the Best Option?
While beneficial for many, pump therapy is not a one-size-fits-all solution.
- Dislike of being attached to a device: A primary concern for some is the constant attachment to a device. If the thought of wearing a pump 24/7 causes significant stress or discomfort, it may not be the right choice.
- Unwillingness to perform frequent blood sugar checks: Successful pump use requires frequent blood sugar monitoring, either with a meter (at least 4 times a day) or a continuous glucose monitor (CGM). Without this data, a pump cannot be used safely or effectively.
- Lack of a strong support system: Having supportive family or caregivers is important, especially for younger users or those who need help with diabetes tasks.
- Significant cost or insurance barriers: The high initial and ongoing costs can be a major obstacle. While ProMed DME works with most insurance plans to minimize expenses, it's a factor to weigh carefully.
- History of non-adherence to diabetes care: Pump therapy requires consistent self-management, including regular site changes and carb counting. A history of non-adherence could increase the risk of complications like DKA.
- Physical or sensory challenges: Severe dexterity issues, vision impairment, or skin allergies to adhesives could make managing a pump difficult.
It's perfectly okay if a pump isn't your ideal choice. Many people achieve excellent diabetes management with other methods. The goal is to find the approach that best supports your health and lifestyle.
Conclusion: Partnering with Your Doctor to Decide

Making the decision about insulin pump therapy isn't something you should do alone. The advantages and disadvantages of insulin pump therapy we've explored represent real trade-offs. The potential for better blood sugar control, reduced hypoglycemia, and greater lifestyle flexibility can be life-changing, but the financial commitment, constant device attachment, and learning curve are equally real considerations.
This is a deeply personal choice. What feels like freedom to one person might feel like a burden to another. For example, a person with a highly variable schedule might find a pump offers needed flexibility, while another who engages in frequent contact sports or swimming might prefer injections to avoid managing a device.
Your healthcare team is your most valuable resource in this decision. Your endocrinologist understands your medical history and can help you assess if the benefits align with your health goals. A certified diabetes educator can walk you through the day-to-day realities of pump therapy.
Take your time with this decision. Ask questions, connect with other pump users if possible, and honestly evaluate your readiness. Choosing not to use a pump doesn't mean you're missing out; many people achieve excellent control with other methods.
Here at ProMed DME, we understand that diabetes management is more than just choosing a device. Whether you opt for pump therapy or continue with injections, you need reliable, high-quality supplies. Based in Stuart, Florida, we ship diabetes supplies across the United States and work with most insurance plans to keep your costs manageable. Our dedicated nurse is available to answer questions, and we believe managing diabetes should be as stress-free as possible.
Whatever path you choose, we're here to support you with the supplies and expertise you need. Contact our team for your diabetes supply needs – because the right decision is the one that works best for you.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.



