Your Guide to Medicare Coverage for Catheter and Urological Supplies

Understanding Medicare Coverage for Your Essential Catheter Supplies
Catheter supplies medicare coverage can feel overwhelming, but the basics are straightforward. Medicare Part B covers catheter supplies as durable medical equipment when they're medically necessary for permanent urinary conditions lasting at least 3 months.
Quick Coverage Overview:
- Intermittent catheters: Up to 200 per month plus sterile lubricant
- Indwelling catheters: Typically 1 per month
- External catheters: Up to 35 per month for men
- Coverage requirement: Permanent urinary incontinence or retention
- Cost: Medicare pays 80% after you meet your Part B deductible
- Documentation needed: Doctor's prescription and medical records
If you're one of the millions of Americans dealing with urinary incontinence or retention, you're not alone. These conditions affect your daily life, but Medicare recognizes catheter supplies as essential medical equipment - not luxury items.
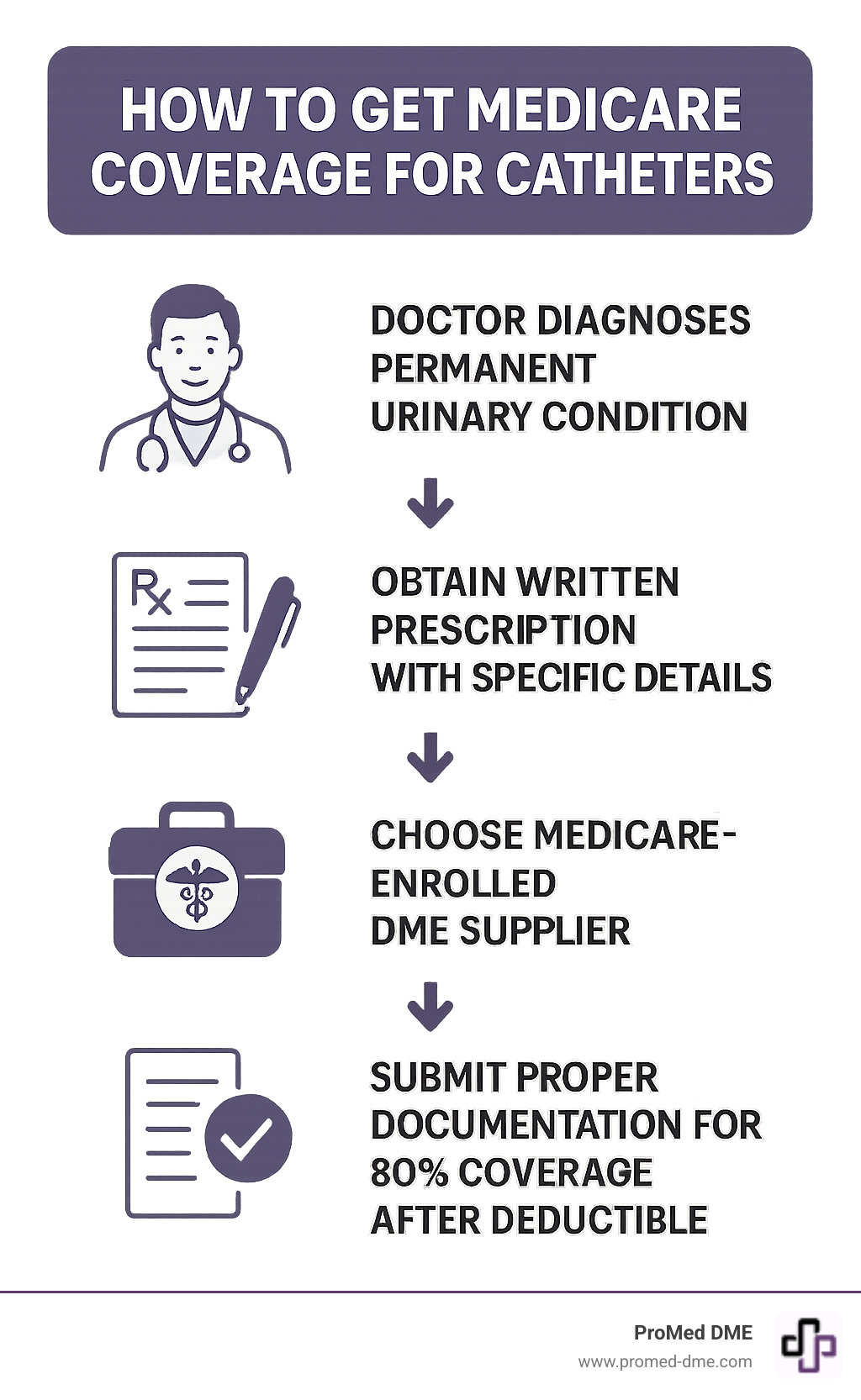
The key to getting your supplies covered lies in understanding three critical elements: medical necessity, proper documentation, and working with Medicare-approved suppliers. Your doctor must certify that your condition is permanent (expected to last at least 3 months) and document why catheters are medically necessary for your specific situation.
Medicare classifies catheter supplies under the Prosthetic Device benefit, which means they're treated as equipment that replaces a body function rather than just convenience items. This classification is important because it determines how your coverage works and what documentation you'll need.
Quick catheter supplies medicare definitions:
- does medicare cover durable medical supplies
- medical supplies medicare covers
- medicare approved durable medical equipment
Understanding Medicare Eligibility for Catheter Supplies
Getting catheter supplies medicare coverage doesn't have to feel like cracking a secret code. The truth is, Medicare wants to help people who genuinely need these supplies - they just need to make sure the coverage goes to the right people for the right reasons.
Think of Medicare's approach like a caring friend who wants to help but needs to understand your situation first. The foundation of all catheter supplies medicare coverage comes down to one key concept: medical necessity. This simply means your doctor has determined that catheters aren't just helpful for you - they're essential for managing your health condition.
Medicare covers catheter supplies under what's called the Prosthetic Device benefit. Now, you might think "prosthetic" only refers to artificial limbs, but Medicare sees it differently. Since catheters replace your body's natural ability to control urination, they're considered prosthetic devices that restore a vital body function.
As stated by the Centers for Medicare and Medicaid Services (CMS), urological supplies like catheters are covered when they're necessary for people with permanent impairment of urination. The good news? Medicare Part B handles this coverage, treating your catheter supplies as durable medical equipment that helps you manage your daily life.
What Are the Core Eligibility Requirements?
Let's break down what Medicare needs to see before they'll cover your catheter supplies. These requirements aren't roadblocks - they're simply Medicare's way of ensuring coverage reaches people who truly need it.
Permanent urinary incontinence or retention tops the list. Your condition needs to be considered long-lasting, which Medicare defines as lasting at least three months. Don't worry - this doesn't mean your situation can never improve, just that it's not expected to resolve quickly.
Your doctor's prescription serves as your golden ticket to coverage. This isn't just a casual note from your physician. Medicare needs a detailed "Plan of Care" that spells out exactly which type of catheter you need, how many you'll use each month, and why they're necessary for your specific condition.
The medically necessary requirement means your doctor's records must paint a clear picture of your medical situation. They need to document your diagnosis, explain how severe your condition is, and describe how catheters will help you manage it effectively.
In-home use is another key factor. Medicare Part B covers supplies you'll use at home, which is different from catheters used during hospital stays (those fall under Medicare Part A coverage).
Finally, you'll need to work with a Medicare-enrolled supplier who accepts Medicare assignment. This is where companies like ProMed DME come in - we handle the Medicare paperwork and billing process, so you can focus on your health instead of insurance hassles.
How Medicare Defines 'Permanent Impairment'
The word "permanent" might sound scary, but Medicare's definition is more flexible than you might expect. They're not necessarily talking about a lifetime condition - they're looking at whether your urinary issues are long-term and unlikely to resolve quickly.
Medicare uses what's often called the 3-month rule. If your doctor believes your condition won't be medically or surgically corrected within three months, it meets Medicare's definition of permanent. This makes sense when you think about it - conditions like neurogenic bladder, spinal cord injuries, or severe incontinence that hasn't responded to other treatments typically require ongoing management.
Your doctor needs to document that your condition has an indefinite duration and represents a chronic diagnosis. This doesn't mean giving up hope for improvement - it simply recognizes that you need reliable access to catheter supplies while managing your condition, whether that's for months, years, or longer.
This practical approach ensures that people with genuine, ongoing needs can get their catheter supplies medicare coverage without jumping through hoops every few weeks to prove they still need help.
What Types of Catheter Supplies Medicare Covers
When it comes to catheter supplies medicare coverage, it's not a one-size-fits-all situation. Medicare covers various types of catheters and associated supplies, each with its own guidelines and quantity limits, depending on your medical needs.

Think of catheter coverage like choosing the right tool for the job. Your doctor will determine which type works best for your specific condition, and Medicare follows their lead. The three main categories are indwelling catheters (like Foley catheters that stay in place), intermittent catheters (straight catheters you use several times a day), and external catheters (condom-style catheters for men and newer external options for women).
Each type serves different medical needs and comes with different quantity limits. Medicare recognizes that someone using intermittent catheters multiple times daily needs more supplies than someone with an indwelling catheter that gets changed monthly. This is why the coverage amounts vary so much between types.
Beyond the catheters themselves, Medicare also covers essential catheter accessories like drainage bags, leg bags, extension tubing, and sterile lubricant packets. These aren't extras - they're necessary components that make catheter use safe and effective.
| Catheter Type | Description | Typical Medicare Coverage (Part B) |
|---|---|---|
| Indwelling | Foley catheters that remain in the bladder | 1 per month plus drainage supplies |
| Intermittent | Single-use straight catheters | Up to 200 per month plus lubricant |
| External | Condom catheters and female external devices | Up to 35 per month for men |
Coverage Differences for Indwelling, Intermittent, and External Catheters
The coverage differences between catheter types reflect how they're actually used in daily life. Foley catheters are indwelling devices that typically stay in place for weeks at a time, so Medicare covers one catheter per month along with the drainage bags and tubing you'll need.
Intermittent catheters work completely differently. These straight-tip catheters are used multiple times throughout the day for sterile-use catheterization. Since you might need to catheterize yourself four to six times daily, Medicare allows up to 200 intermittent catheters per month. This generous monthly allowance ensures you never have to reuse a catheter, which could lead to dangerous infections.
External catheters offer another approach entirely. Condom catheters for men are designed to be changed daily, so Medicare typically covers up to 35 per month. The newer female external catheters are also gaining coverage, though the approval process may require additional documentation since they're relatively new to the market.
Each type requires different supporting supplies too. Intermittent catheter users need sterile lubricant packets, while indwelling catheter users need various drainage bags and leg straps to secure everything comfortably.
Special Catheter Coverage: Coudé and Closed-System Catheters
Sometimes standard catheters just won't work for your specific anatomy or medical condition. That's where specialized catheters come in, and Medicare does cover them - but you'll need stronger medical justification.
Coudé tip catheters have a curved tip that makes insertion easier for people with enlarged prostates or urethral strictures. Your doctor needs to document why a standard straight catheter won't work for you. This Coudé tip justification typically involves anatomical reasons that make standard catheterization difficult or impossible.
Closed-system catheters are the premium option for people at high risk of urinary tract infections. These pre-lubricated, sterile systems reduce infection risk significantly. Medicare covers them for specific conditions including recurrent UTIs, immunosuppression, and spinal cord injury.
The conditions that typically qualify for closed-system catheter coverage include people with compromised immune systems, those with a history of frequent UTIs despite proper catheter technique, individuals with spinal cord injuries, and patients with other conditions that put them at exceptionally high risk for complications. Your doctor will need to provide detailed medical documentation explaining why standard intermittent catheters aren't sufficient for your safety.
Covered Quantities and Associated Supplies
Medicare's quantity limits aren't arbitrary numbers - they're based on medical best practices and typical usage patterns. The up to 200 intermittent catheters per month allows for multiple daily catheterizations while maintaining sterility. This quantity ensures you never have to choose between proper hygiene and running out of supplies.
Along with the catheters themselves, Medicare covers essential supplies that make catheterization safe and comfortable. Lubrication packets are covered for intermittent catheter users because proper lubrication prevents injury and makes the process more comfortable. Drainage bags come in different sizes - overnight bags that hold more urine and smaller leg bags for daytime discretion.
Extension tubing and leg straps might seem like small details, but they're crucial for maintaining an active lifestyle with an indwelling catheter. These supplies help secure everything properly while allowing you to move around comfortably.
Medicare Part B covers these supplies at 80% after you meet your deductible, just like other durable medical equipment. At ProMed DME, we handle all the insurance paperwork and work directly with Medicare to minimize your out-of-pocket costs. Our team understands exactly what documentation Medicare requires, so you can focus on your health rather than paperwork hassles.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.