Continuous Glucose Monitors for Type 2: Sweet Tech or Bitter Pill?
Understanding Continuous Glucose Monitors for Type 2 Diabetes
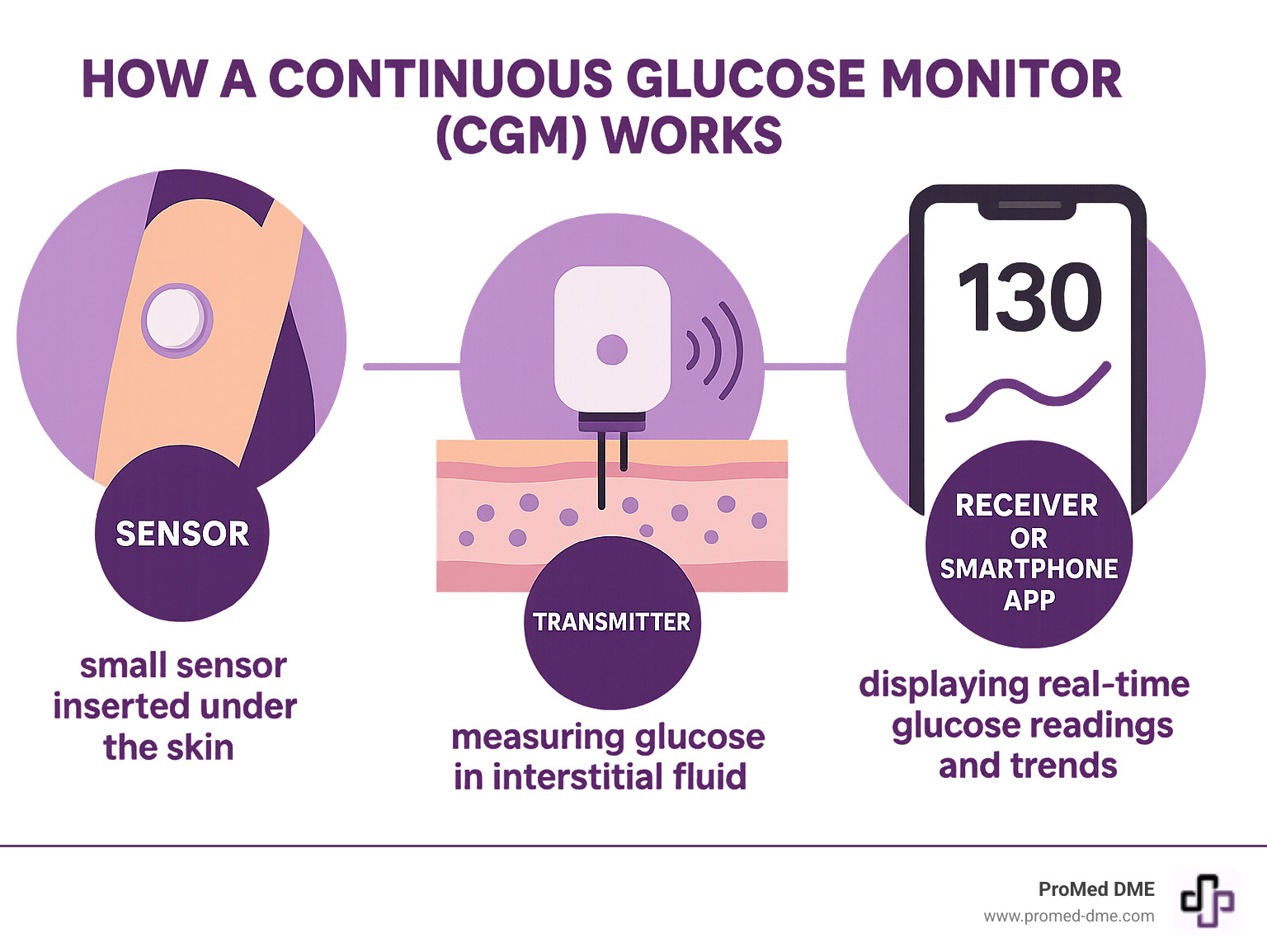
CGM for type 2 refers to using a Continuous Glucose Monitor to track blood sugar levels in people with Type 2 Diabetes. This small, wearable device provides real-time glucose readings, replacing the guesswork of traditional finger pricks with a constant stream of data. It helps users see exactly how diet, exercise, and medication affect their blood sugar, leading to more informed choices and better management.
Continuous Glucose Monitors (CGMs) are changing the game for many people with type 2 diabetes. But is this technology a game-changer for everyone, or does it come with challenges like cost and access?
This guide will explore how CGMs work, who benefits most, and what the future holds for this vital technology to help you decide if a CGM is the right tool for your diabetes journey.
Basic CGM for type 2 glossary:
The Power of Data: Key Benefits of CGM for Type 2 Diabetes
Managing diabetes with traditional finger-prick tests is like navigating a city with only a few random photos. Continuous Glucose Monitors (CGMs) provide a real-time GPS of your glucose levels, allowing you to see trends, patterns, and the immediate impact of your choices.
For individuals with CGM for type 2, this continuous data translates into significant benefits. Studies show that using a CGM can lead to a meaningful drop in HbA1c (your three-month average blood sugar). This means better long-term glucose control, which is crucial for preventing diabetes complications.
Beyond a lower A1c, CGMs provide dynamic data that changes the game:
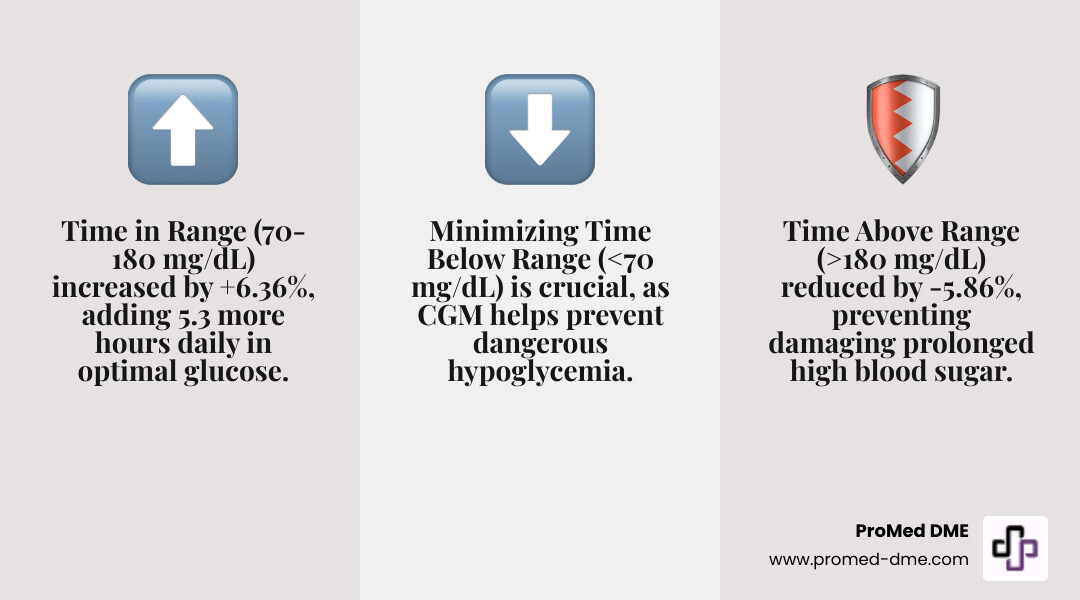
- Improved Time in Range (TIR): CGM users spend more time in their ideal glucose zone (70-180 mg/dL), with studies showing an increase of over 6%. That's more than 5 extra hours a day in your target range.
- Less Time in Highs and Lows: The data shows a significant decrease in Time Above Range (>180 mg/dL) and helps prevent dangerous low blood sugar (hypoglycemia) by providing alerts when your glucose is trending down.
- Powerful Behavior Modification: This is a key benefit of CGM for type 2. Seeing how a meal or a walk immediately impacts your glucose is incredibly motivating. This instant feedback helps you make smarter food and activity choices, turning guesswork into an informed strategy. You can pinpoint which foods cause spikes and see how exercise helps stabilize your levels.
- Fewer Finger Pricks: While some calibration checks may be needed depending on the device, the need for constant, painful finger pricks is dramatically reduced.
- Proactive Adjustments: Instead of reacting to symptoms, you can see trends and make small adjustments throughout the day, like taking a short walk after a meal to prevent a spike. This reduces diabetes-related anxiety and provides a sense of control.
Scientific research on CGM effectiveness
Understanding Key CGM Metrics
CGMs introduce several new metrics that provide a richer picture of your glucose control beyond the three-month HbA1c average:
- Time in Range (TIR): The percentage of time your glucose is within a target range (typically 70-180 mg/dL). The goal for most is >70%.
- Time Below Range (TBR): The percentage of time your glucose is below 70 mg/dL. This indicates time spent in or at risk of hypoglycemia.
- Time Above Range (TAR): The percentage of time your glucose is above 180 mg/dL. This indicates time spent in hyperglycemia.
- Glucose Management Indicator (GMI): An estimate of your HbA1c based on your CGM data, giving you a snapshot of your long-term control without a lab test.
These metrics, combined with real-time trend data, empower you and your doctor to fine-tune your diet, exercise, and medication. This continuous feedback loop transforms diabetes management from abstract advice into actionable, personal insights.
Is a CGM Right for You? Who Benefits Most
Wondering if a CGM for type 2 diabetes is right for you? The technology is no longer just for those with type 1 or on intensive insulin. We now know that many of the nearly 80% of people with type 2 diabetes who don't use insulin can still have unnoticed blood sugar swings.
If you've ever wanted to see how a specific meal or activity truly affects your blood sugar, a CGM might be what you need. Let's break down who benefits most.
For Those on Insulin Therapy
A CGM for type 2 can be a game-changer if you use insulin, especially basal insulin or multiple daily injections. Research shows people on basal insulin who use CGMs see a significant reduction in A1c levels compared to those who don't. The key benefit is preventing hypoglycemia (low blood sugar), as the device can alert you to falling glucose levels before they become dangerous. CGMs also provide the detailed data needed to accurately titrate insulin doses, removing the guesswork from adjustments.
Evidence from the ADA/EASD consensus report
The Growing Case for CGM for type 2 Without Insulin
The conversation is evolving for people managing diabetes with diet, exercise, and oral medications. For this group, a CGM acts like a personal diabetes coach, providing immediate feedback on how food choices and activity impact blood sugar. Seeing a glucose spike after a certain food is a powerful motivator for change.
A CGM can reveal hidden glucose spikes after meals that you might not feel but which can cause damage over time. For the newly diagnosed, using a CGM can guide early lifestyle changes that may delay or prevent the need for medication. With about 80% of type 2 patients not using insulin, millions could benefit from the self-management insights a CGM provides.
More info about diabetes supplies
In short, a CGM may be a great tool if you are on any insulin therapy, experience frequent or undetected lows, have a high or fluctuating A1c, or are motivated to use real-time data to optimize your lifestyle choices and take a more active role in your health.
CGM vs. Traditional Finger Pricks: A Clearer Picture
Managing diabetes with traditional finger-prick meters (SMBG) is like seeing a few still photos of a movie—you get snapshots, but miss the full story. Using a CGM for type 2 is like upgrading to a real-time video of your glucose levels.
Here’s a quick comparison:
| Feature | Continuous Glucose Monitoring (CGM) | Self-Monitoring of Blood Glucose (SMBG) (Finger Pricks) |
|---|---|---|
| Frequency | Continuous (every 1-5 minutes) | Intermittent (typically 1-8 times per day) |
| Data Type | Real-time trends, patterns, and numeric values | Single numeric value at time of test |
| Trend Visibility | Shows rising, falling, and stable glucose; predictive alerts | Only shows current glucose; no trend information |
| Actionability | Proactive adjustments based on trends; prevents highs/lows | Reactive adjustments based on single reading |
| Comfort/Convenience | Less invasive (sensor changed every 10-14 days); no daily pricks | Requires daily finger pricks; can be painful/inconvenient |
| Insights | Reveals impact of food, exercise, stress, sleep on glucose patterns | Provides limited insight into glucose fluctuations throughout the day |
Even your HbA1c, a three-month average, can be misleading. Two people can have the same HbA1c but vastly different daily glucose patterns—one stable, the other a roller-coaster of highs and lows. A CGM reveals this entire journey.
CGM provides dynamic data, showing the peaks, valleys, and rate of change. This is crucial because high glucose variability is linked to long-term complications. Finger pricks provide static data—a single point in time with no context. This shift from reacting to a number to proactively managing a trend is a key advantage of CGM for type 2. You can see a post-meal rise and take a walk to manage it, or see a downward trend and have a snack to prevent a low. This level of insight and control isn't possible with finger pricks alone.
Navigating Problems: Cost, Coverage, and Limitations
While the benefits of CGM for type 2 are clear, practical problems like cost and insurance coverage exist. Without insurance, the yearly cost can range from $2,500 to $6,000, with sensors alone costing $120 to $200 per month.
Insurance Coverage and Access
Access often depends on your insurance plan, and rules can be complex.
- Medicare has traditionally covered CGMs for those on intensive insulin therapy, but coverage is expanding to include more people with diabetes.
- Medicaid coverage can vary, and disparities in access are a concern. Advocacy groups are working to ensure fairer, more consistent coverage for all who could benefit.
- Private Insurance plans typically require a prescription and may have specific criteria based on insulin use, history of hypoglycemia, or A1c levels. A "letter of medical necessity" is often required. A supplier like ProMed DME can help steer this process to minimize your out-of-pocket costs.
Prescription Process
You will need a prescription to get a CGM. While endocrinologists have historically prescribed most CGMs, primary care physicians (PCPs) are increasingly getting involved, which helps improve access.
Understanding the Downsides of CGM for type 2
Beyond cost and paperwork, there are other factors to consider:
- Alarm Fatigue: Constant alerts for high or low glucose can become tiresome, leading some to ignore them.
- Sensor Adhesion Issues: The sensor must stick to your skin for 10-14 days. Some people experience skin irritation or find the sensor gets knocked off accidentally.
- Information Anxiety: The sheer volume of data can feel overwhelming or lead to an unhealthy focus on every number. It's important to focus on overall trends.
- Calibration Requirements: While many newer CGMs are factory-calibrated, some models may still require occasional finger-prick tests to ensure accuracy.
- Lag Time: CGMs measure glucose in the fluid between cells, not blood, so there's a 5- to 15-minute delay compared to a finger-prick reading. This is important to remember when glucose levels are changing rapidly.
- Learning Curve: It takes time to get comfortable applying the sensor, using the app, and interpreting the data.
Despite these considerations, many find the benefits of real-time insight and improved control far outweigh the potential drawbacks.
The Future is Continuous: CGMs in Primary Care
Continuous Glucose Monitors (CGMs) are helping to create a future where diabetes management is a more supported journey, especially within primary care. In the past, treatment adjustments were often delayed due to a lack of data between appointments—a problem known as "therapeutic inertia."
CGM for type 2 helps solve this by providing a constant stream of glucose insights. This allows your primary care physician (PCP) to get a clear picture of your glucose patterns and make more timely, informed decisions. While specialists have traditionally been the main prescribers, PCPs are increasingly prescribing CGMs. In fact, studies show that CGM use managed in a primary care setting leads to significant A1c reduction for people with type 2 diabetes.
Modern CGM for type 2 systems make it easy to share your data with your healthcare team, making appointments more productive. You and your doctor can review trends together, focusing on what's working. The rise of telemedicine and virtual diabetes clinics also leverages CGM data for remote monitoring and personalized guidance, expanding access to expert care.
By providing continuous data and encouraging proactive management, CGMs are leading to significantly improved health outcomes. The trend is clear: as prescribing by PCPs grows, this essential tool is becoming more accessible, shaping a more connected and effective future for diabetes care.

Frequently Asked Questions about CGMs for Type 2 Diabetes
Making the switch to a CGM can bring up a lot of questions. Here are answers to the most common concerns about CGM for type 2.
Does wearing a CGM hurt?
Most people are pleasantly surprised by how little they feel it. The sensor insertion is done with a spring-loaded applicator that places a tiny, flexible filament under the skin in a split second. The filament is very thin, and once it's in place, the vast majority of users forget it's there. You can shower, sleep, and go about your daily activities normally.
Proper skin preparation (cleaning and drying the area) helps the sensor stick well and reduces the risk of irritation. While some people may have mild adhesive sensitivity, solutions like barrier wipes are available. For most, the initial worry about pain disappears after the first application.
Do I still need to do finger-prick tests with a CGM?
The need for finger pricks is dramatically reduced, but they are still useful in certain situations. Many modern CGMs are factory-calibrated and don't require routine finger sticks. However, it's wise to use a traditional meter for:
- Confirming highs and lows: If your CGM gives an extreme reading that doesn't match how you feel, a finger prick can confirm the number. This is especially true in the first 24 hours of a new sensor.
- Symptom mismatch: If you feel the symptoms of low blood sugar but your CGM reads normal, trust your body and double-check.
Calibration requirements vary by device, so always follow the manufacturer's instructions and your doctor's advice. Think of your CGM as your primary tool and your meter as a reliable backup.
How do I get a CGM for my Type 2 diabetes?
Getting a CGM for type 2 starts with a conversation with your doctor to get a prescription. Your provider will determine if a CGM is medically appropriate for your situation.
Once you have a prescription, the next step is often insurance pre-authorization, which can be complex. This is where an experienced Durable Medical Equipment (DME) supplier like ProMed DME is invaluable.
We handle the insurance paperwork for you. Our team works with most insurance plans, and we have a dedicated nurse on staff who specializes in managing the documentation to meet your insurer's requirements. We know what information they need and how to present it to minimize your out-of-pocket costs.
We can help you check your eligibility upfront to understand your plan's specific requirements. At ProMed DME, we ship across the United States and offer free shipping directly to your door. Our goal is to handle the complexities so you can focus on your health.
Conclusión
Managing type 2 diabetes has been transformed by CGM for type 2 technology. It represents a fundamental shift from reactive guesswork to proactive, informed health management. By providing a continuous view of your glucose levels, CGMs show you exactly how diet, exercise, and medication affect your body in real time.
The evidence is clear: CGM users see significant improvements in Time in Range, lower HbA1c levels, and a deeper understanding of their own glycemic patterns. While challenges like cost and insurance navigation exist, the benefits of control and peace of mind are often life-changing.
A CGM is a powerful tool, not a magic wand. It provides the insights, but you make the choices. With better information comes the power to achieve better outcomes.
At ProMed DME, we've seen how CGMs empower people. Our dedicated nurse helps steer insurance requirements, we work with most plans to keep your costs down, and we ship supplies with free shipping directly to your door. We're here to support your journey toward better health.
Ready to get a clearer picture of your diabetes management? The data is waiting to tell your story.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.




