Getting Started with Pump Therapy: Calculating Your Basal Insulin

Why Getting Your Basal Insulin Right Is Critical for Pump Success
How much basal insulin when starting pump therapy depends on your current insulin needs, but here's the quick answer most people need:
Starting Basal Insulin Calculation:
- Calculate your Total Daily Dose (TDD) - Add up all insulin from the past 4 days, then divide by 4
- Reduce by 25-30% for pump therapy (multiply by 0.7-0.75)
- Take 50% for basal insulin (the other 50% becomes bolus insulin)
- Divide by 24 hours to get your starting hourly basal rate
Example: If your TDD was 40 units → 40 × 0.75 = 30 units pump TDD → 15 units daily basal ÷ 24 = 0.6 units/hour starting rate
Starting pump therapy is a major shift in diabetes management. Instead of fixed long-acting shots, your pump delivers tiny, adjustable amounts of rapid-acting insulin every few minutes. This precision makes getting your basal rates right from day one essential.
Research shows basal insulin should be about 40-50% of your total daily insulin needs. However, initial calculation formulas can overestimate this amount. Studies find many patients need less basal insulin than calculated, especially when aiming for tight glucose control.
You don't need to figure this out alone. Your diabetes care team will help calculate and adjust your doses. Most people need 3-5 different basal rates to account for hormone changes, and it takes about 3-5 months to get them dialed in.
How much basal insulin when starting pump therapy vocab to learn:
- aace guidelines for insulin pump therapy
- advantages and disadvantages of insulin pump therapy
- continuous glucose monitoring system
Understanding Basal Insulin: The Pump Advantage
If you use daily injections, you're familiar with basal insulin. It's the steady, background insulin that works 24/7 to keep blood sugar stable between meals and overnight, covering the glucose your liver naturally produces.
Basal insulin is different from bolus insulin, which is the "meal-time" insulin you take to cover carbohydrates or correct high blood sugar. While bolus insulin handles the spikes, basal insulin keeps everything steady. For people with type 1 diabetes especially, getting basal insulin right is crucial - without it, there's a real risk of diabetic ketoacidosis (DKA).
MDI vs. Pump Delivery: A Game Changer
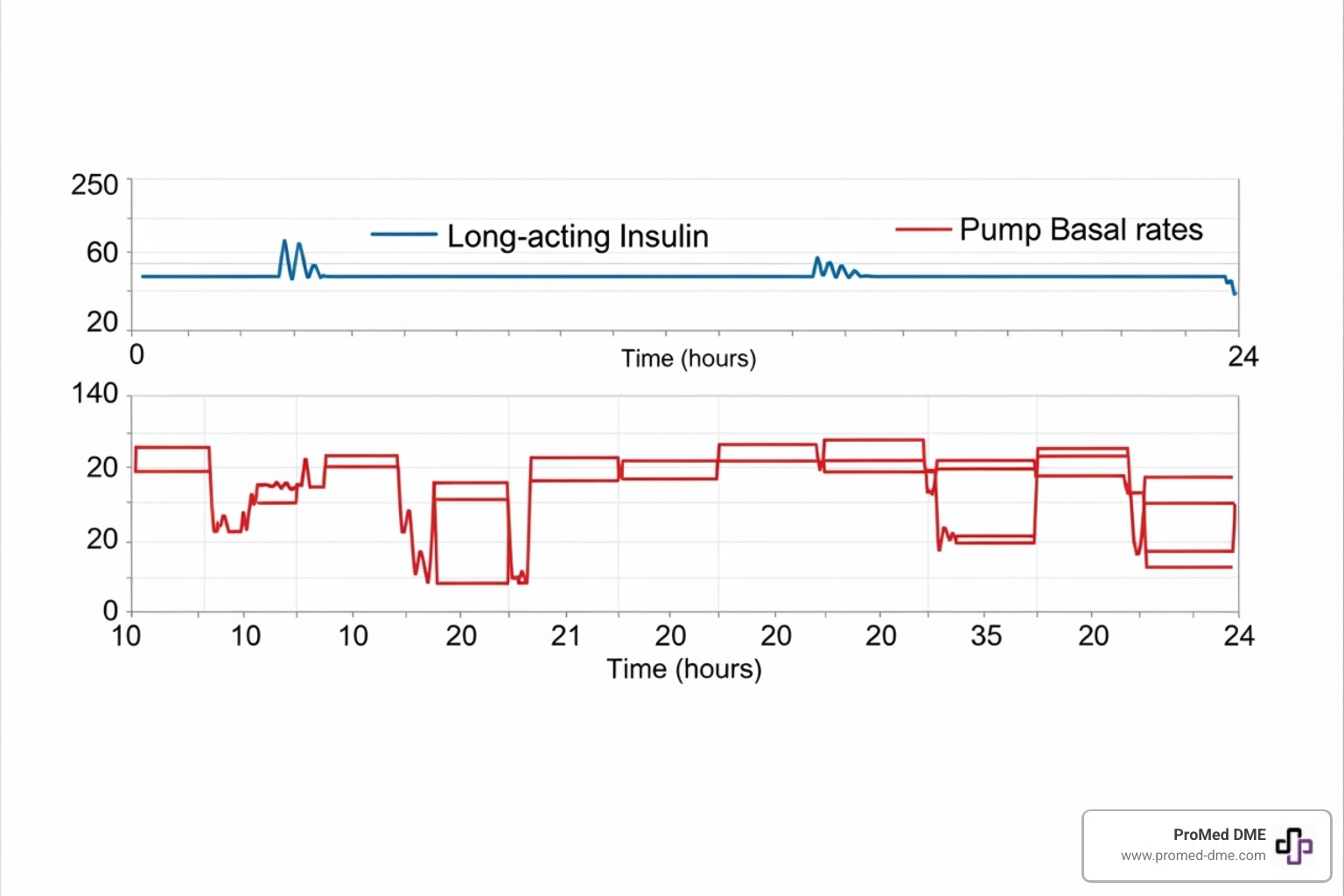
With injections, you likely use a long-acting insulin like Lantus or Tresiba. These work well, but they're inflexible; once injected, the dose works for 12-24 hours, regardless of changes in your needs.
When figuring out how much basal insulin when starting pump therapy, everything changes. Your pump only uses rapid-acting insulin for both basal and bolus delivery. Instead of one big injection, your pump delivers tiny amounts every few minutes through a small cannula under your skin.
This continuous infusion is measured in units per hour. Instead of injecting 20 units of long-acting insulin once a day, you might program your pump to deliver 0.8 units every hour. The delivery method gives you incredible flexibility and precision.
You can program different basal rates throughout the day. For example, you might need a higher rate in the morning to handle the dawn phenomenon. Your pump manages this automatically, and most people use 3-5 different rates to match their body's rhythms.
Modern pumps can deliver insulin in incredibly small amounts—often as little as 0.05 units per hour. This level of precision isn't possible with injections and allows for truly personalized diabetes management.
The result is better blood sugar control with fewer highs and lows, plus the freedom to adjust your insulin delivery. It's a significant upgrade that mimics how a healthy pancreas works.
How to Calculate How Much Basal Insulin When Starting Pump Therapy
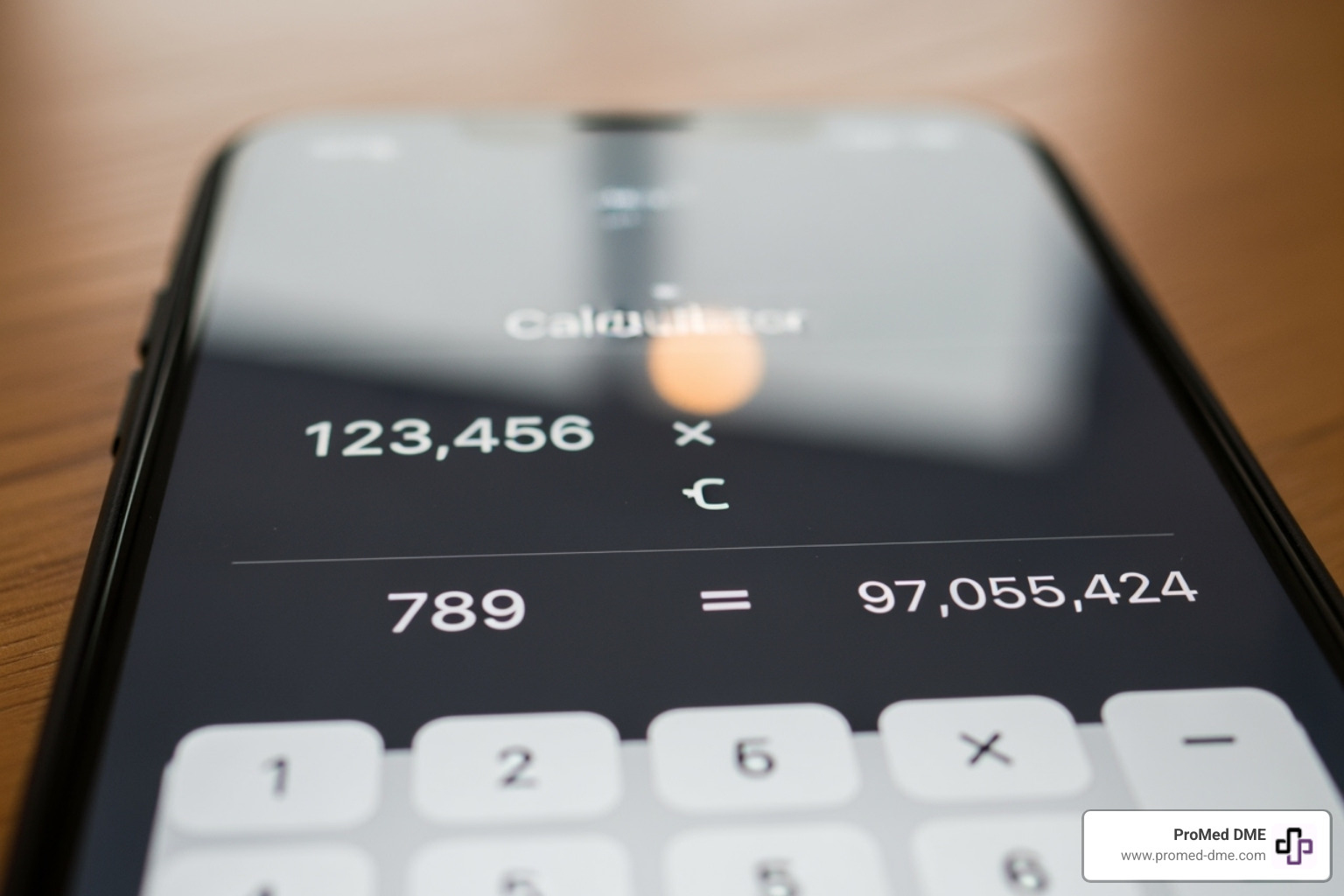
The math for how much basal insulin when starting pump therapy might seem intimidating, but it's a straightforward process using your current insulin needs as a starting point.
Everything starts with your Total Daily Dose (TDD): all the insulin you use in a 24-hour period (long-acting, mealtime, and correction doses). TDD is a safe and reliable starting point for estimating pump doses for both type 1 and type 2 diabetes.
When switching to a pump, your total daily insulin is typically reduced. Because pump-delivered rapid-acting insulin is used more efficiently by the body, most healthcare teams reduce the MDI total by 25-30% for the initial pump settings.
Once you have your new pump TDD, you split it. About 50% goes to basal insulin (your background needs), and the other 50% covers your bolus insulin. This ratio can be adjusted based on your diet and lifestyle.
The final step is dividing your daily basal amount by 24 to get your starting hourly rate.
Example Calculation:Say your average Total Daily Dose on injections was 50 units. Here's how the math works: First, we reduce that by 25%, so 50 × 0.75 = 37.5 units for your new pump TDD. Next, we take half for basal insulin: 37.5 × 0.50 = 18.75 units of basal per day. Finally, we divide by 24 hours: 18.75 ÷ 24 = 0.78 units per hour as your starting basal rate.
That 0.78 units per hour would be programmed as a flat rate initially, though most people eventually need different rates throughout the day.
A Step-by-Step Guide for How Much Basal Insulin When Starting Pump Therapy
Ready to crunch some numbers? Your diabetes team will double-check everything, but understanding the process helps you feel more confident. Let's break down how much basal insulin when starting pump therapy into bite-sized steps.
Step 1 involves calculating your current Total Daily Dose. The key is getting an accurate average. Add up all your insulin from the past four days—every long-acting shot, mealtime dose, and correction. Then divide that total by four.
Step 2 accounts for pump efficiency by reducing your TDD. Multiply your average daily dose by 0.75 (a 25% reduction). Most teams start conservatively to avoid low blood sugars.
Step 3 determines your total daily basal dose by taking that reduced TDD and cutting it in half. This 50-50 split between basal and bolus insulin works well for most people but can be adjusted by your team.
Step 4 gives you your starting hourly rate by dividing your daily basal total by 24 hours. This flat rate serves as your foundation, which you'll fine-tune over the coming months.
Key Factors Influencing How Much Basal Insulin When Starting Pump Therapy
While the TDD calculation is a solid starting point, several unique factors influence your final basal insulin needs. This explains why rates differ between people, even with similar TDDs.
Body weight plays a significant role. General guidelines suggest starting doses around 0.1-0.2 units per kilogram of body weight. However, your individual insulin sensitivity is just as important.
Insulin sensitivity varies dramatically. Some people need very little insulin, while others require more to get the same results. Your healthcare team will assess your sensitivity by observing how your blood sugar responds to insulin.
Your carbohydrate intake also shifts the basal-to-bolus balance. If you follow a low-carb lifestyle, you might need more than 50% of your insulin as basal. Conversely, a high-carb diet may require less basal and more bolus insulin.
The dawn phenomenon is a common reason for multiple basal rates. Between 3 AM and 8 AM, your body releases hormones that raise blood sugar. Many pump users need a higher basal rate during these hours to counteract this.
Your lifestyle and activity levels are also key. Exercise typically lowers insulin needs, while stress or illness can increase them. Pump therapy allows you to adjust basal rates to match these variations, offering flexibility injections can't.
Fine-Tuning Your Doses: Basal Rate Testing and Adjustments
Starting pump therapy is like learning to drive a new, highly sophisticated car – you get the basics down, but true mastery comes with practice and fine-tuning. Getting your basal rates just right is a process that requires patience, observation, and close collaboration with your diabetes care team.
Patience and Process
We understand the excitement of starting a pump and wanting perfect blood sugars overnight. However, it's important to set realistic expectations. Setting and adjusting basal insulin in pump therapy takes more time and work than injections. It can take anywhere from 3 to 5 months or even more to truly dial in your rates. This isn't a sign of failure; it's a normal part of the process. We're mimicking a complex biological system!
Basal Rate Testing
The cornerstone of fine-tuning your basal rates is basal rate testing. This involves fasting (or skipping meals) during specific time blocks while watching your blood glucose. The goal is to see how your blood sugar behaves when it's solely influenced by your basal insulin, without the impact of food or bolus insulin.
Here’s how it generally works:
- Overnight Testing: This is often the first and most crucial test. You'll typically fast from dinner until breakfast, checking your blood sugar at regular intervals (e.g., 12 AM, 3 AM, 6 AM). The aim is to see stable glucose readings that don't change by more than 30 mg/dL over the test period. If your blood sugar drifts up or down significantly, it indicates your overnight basal rate needs adjustment.
- Daytime Testing: For daytime basal rates, you'll test specific blocks of time, often by skipping a meal. For example, you might skip breakfast and monitor your blood sugar from morning to lunchtime, or skip lunch and monitor from lunchtime to dinner. During these tests, it's crucial not to eat or take any correction boluses for high blood sugars, as this would interfere with evaluating your basal rate.
Stable Glucose Goal
During basal rate testing, what are we looking for? Stability! We want your blood glucose to remain relatively flat, not rising or falling dramatically. If your glucose level decreases by more than 30 mg/dL or falls below your target, it's a sign that your basal rate for that period might be too high and needs to be decreased by 10-20%. Conversely, if your glucose rises by more than 30 mg/dL, your basal rate might be too low and needs to be increased by 10-20%.
Circadian Profiles and the Dawn Phenomenon
Most people on pump therapy will program 3 to 5 different basal rates over 24 hours. This "circadian profile" acknowledges that our insulin needs aren't constant. For instance, many individuals experience the "dawn phenomenon," requiring a higher basal rate in the early morning hours (e.g., 2 AM to 8 AM) to prevent rising blood sugars. Your pump allows us to precisely increase insulin delivery during these specific times and then lower it again later in the day.
Making Small Changes
When adjusting basal rates, precision is key. We typically make small changes, often in increments of 0.05 or 0.1 units per hour. These tiny adjustments, made over weeks and months, gradually lead to optimal control. It's a continuous learning process, and your needs can change over time due to factors like weight changes, activity levels, or even stress, requiring periodic recalibration.
This is where your diabetes care team shines. They will help you interpret your blood glucose data, especially from your continuous glucose monitor (CGM), to make informed decisions about your basal rate adjustments. If you're looking for support, you can always Find a Diabetes Care and Education Specialist.

Safety and Modern Technology in Basal Management
Starting pump therapy opens up incredible possibilities for diabetes management, but like any powerful tool, it comes with important safety considerations. The good news is that modern technology has made pump therapy safer than ever before, and understanding these safety aspects will help you feel confident in your journey.
Hypoglycemia Risk
One of the biggest adjustments when figuring out how much basal insulin when starting pump therapy is learning to prevent low blood sugar. Since your pump delivers rapid-acting insulin continuously, setting your basal rates too high can lead to frequent hypoglycemia. Unlike those long-acting insulin shots that you can't "un-inject," your pump gives you more control - you can temporarily suspend insulin delivery if needed.
Here's what to watch for: if your blood glucose drops more than 60 mg/dL during a basal test or falls below your target range, that's your body telling you the basal rate is too high for that time period. The solution is usually straightforward - reduce that rate by about 10-20%.
Always keep fast-acting carbohydrates handy. Whether it's glucose tablets, juice, or even regular soda, having a quick source of sugar within reach is essential. Remember the "Rule of 15": consume 15 grams of fast-acting carbs, wait 15 minutes, recheck your blood sugar, and repeat if necessary. It's simple, but it works.
DKA Prevention
For people with type 1 diabetes especially, continuous basal insulin is absolutely critical to prevent diabetic ketoacidosis (DKA). This is one area where pump therapy requires extra vigilance. Since your pump only uses rapid-acting insulin, there's no long-acting "backup" insulin circulating in your system like there was with injections.
If your pump malfunctions, your infusion site fails, or you disconnect for too long, DKA can develop surprisingly quickly - sometimes within just 4 hours. That's why having a solid backup plan is non-negotiable. Keep backup insulin pens, know how to give yourself injections, and don't hesitate to check for ketones if your blood sugar climbs unexpectedly high.
Infusion Site Issues
Your pump's infusion site is like a tiny doorway for insulin delivery, and keeping that doorway clear and healthy is crucial for consistent blood sugar control. Change your infusion site every 2-3 days - this isn't just a suggestion, it's essential for preventing problems.
Using the same spot repeatedly can cause lipohypertrophy (those lumpy fatty deposits under the skin) or scar tissue buildup. When this happens, insulin absorption becomes unpredictable, leading to those frustrating unexplained high blood sugars. Rotate your sites regularly, keep them clean, and your skin will thank you with better insulin absorption.
Importance of CGM
If calculating how much basal insulin when starting pump therapy feels overwhelming, a continuous glucose monitor (CGM) is your best friend. CGM technology has completely transformed how we manage basal insulin by providing real-time glucose readings and showing trends that traditional fingerstick meters simply can't capture.
With a CGM, you can see exactly how your blood sugar responds to your basal insulin throughout the day and night. Those overnight patterns that were once a mystery? Now you can see them clearly. This detailed data makes basal rate testing much more precise and helps you and your healthcare team make informed adjustments rather than educated guesses.
Automated Insulin Delivery (AID) and Hybrid Closed-Loop Systems
The future of diabetes management is already here with Automated Insulin Delivery (AID) systems and hybrid closed-loop technology. These smart systems take much of the guesswork out of basal insulin management by automatically adjusting your insulin delivery based on your CGM readings.
Systems with advanced algorithms can predict where your blood sugar is heading and make tiny adjustments to your basal rates - increasing insulin when you're trending high, decreasing or even suspending delivery when you're heading low. They work tirelessly in the background, like having a diabetes management assistant that never sleeps.
While these systems still require your input for meals and exercise, they significantly reduce the daily burden of constant manual adjustments. They provide an extra layer of safety and convenience that makes living with diabetes feel less overwhelming.
The science behind these systems is fascinating and constantly evolving. For those interested in diving deeper into the research, you can explore Scientific research on automated insulin delivery.
Modern pump therapy has come a long way from the early days, and these technological advances are making diabetes management more precise, safer, and frankly, more liveable than ever before.
Frequently Asked Questions about Starting Basal Insulin on a Pump
We get lots of thoughtful questions from people who are considering or just starting pump therapy. Here are the ones that come up most often about how much basal insulin when starting pump therapy:
How long does it take to get my basal rates right?
Let's be completely honest here - this is a marathon, not a sprint! While your diabetes team will calculate your initial basal rates on pump start day, getting them perfectly tuned takes patience and persistence.
Most people need about 3 to 5 months to get their basal rates truly dialed in, though some may need even longer. This timeline might sound daunting, but you're essentially teaching your pump to mimic what a healthy pancreas does naturally - and that's incredibly complex work!
The process involves careful monitoring with your continuous glucose monitor, doing those basal rate tests we talked about earlier, and making small adjustments with your healthcare team. Think of it as an ongoing conversation between you, your pump, and your diabetes care team. Your body's needs can shift over time due to changes in weight, activity level, stress, or just getting older, so some fine-tuning is always part of the journey.
What's the difference in calculating basal insulin for Type 1 vs. Type 2 diabetes?
Here's some good news - the core principles for calculating how much basal insulin when starting pump therapy are essentially the same whether you have type 1 or type 2 diabetes. We still use your Total Daily Dose (TDD) as our starting point because research shows this method works safely for both groups.
That said, there are some subtle differences worth knowing about. People with type 2 diabetes often deal with varying degrees of insulin resistance, which can influence their overall insulin needs and how their body responds to basal insulin.
For those with type 1 diabetes, both your body weight and your previous long-acting insulin dose help predict your final basal rates. But for type 2 diabetes, typically only your previous long-acting insulin dose matters - weight seems to be less of a factor in determining basal needs for this group.
Regardless of your type of diabetes, the testing and adjustment process is equally important for achieving great blood sugar control. Your diabetes team will work with you to find what works best for your unique situation.
Do I still need to calculate basal rates with a hybrid closed-loop system?
Absolutely! Even if you're using one of those amazing hybrid closed-loop systems that can automatically adjust your insulin, your initial basal rate settings are still the crucial foundation everything else builds on.
Think of your programmed basal rates as the baseline that guides the algorithm. The system's smart features work by making temporary increases or decreases to your basal delivery based on your CGM readings, but it needs those initial settings to know where to start.
If your baseline basal rates are way off from the beginning, even the most sophisticated algorithm will struggle to keep your blood sugars in range effectively. Plus, there are times when you might need to switch back to manual mode - maybe your CGM isn't working properly, or you're doing certain activities where manual control works better.
The technology is incredibly helpful, but understanding your basal rates remains essential for successful pump management. It's like having a really smart co-pilot, but you still need to know how to fly the plane!
Conclusión
Starting insulin pump therapy marks the beginning of a new chapter in your diabetes journey - one filled with more flexibility, precision, and ultimately, freedom. Understanding how much basal insulin when starting pump therapy is your first step toward mastering this incredible technology that can transform how you manage your diabetes.
We've walked through the essential calculation together: taking your Total Daily Dose, reducing it for pump efficiency, splitting it between basal and bolus needs, and arriving at that crucial starting hourly rate. But here's what we want you to remember most - this initial number is just your launching pad, not your final destination.
The real trip begins in those first few months as you and your healthcare team fine-tune your rates. Yes, it takes patience. Yes, there will be some trial and error. But every small adjustment brings you closer to the stable blood sugars and lifestyle flexibility that drew you to pump therapy in the first place. The investment of time and effort in getting your basal rates right pays dividends for years to come.
Your continuous glucose monitor becomes your best friend during this process, showing you exactly how your body responds to different basal rates throughout the day and night. Those overnight graphs that stay beautifully flat? That's the reward for all your careful testing and adjusting.
At ProMed DME, we've seen countless people successfully transition to pump therapy, and we're here to support you through every step of your journey. Our dedicated nurse is always available to answer your questions about supplies, insurance coverage, or just to provide encouragement when the fine-tuning process feels overwhelming. We work with most insurance plans to keep your out-of-pocket costs as low as possible, because we believe everyone deserves access to the best diabetes management tools available.
You're not just learning to use a medical device - you're gaining a partner in diabetes management that can adapt to your life's changing rhythms. Whether you're dealing with dawn phenomenon, planning for exercise, or simply wanting more predictable blood sugars, your pump is there to help.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.



