Insulin Pump Therapy 101 – Your Guide to Easy Diabetes Control

Taking Control of Your Diabetes with Modern Technology
How to use insulin pump therapy starts with understanding the basics. For those looking for a quick guide, here's what you need to know:
- Fill the insulin reservoir with rapid-acting insulin every 2-3 days
- Insert a new infusion set into fatty tissue (abdomen, thigh, buttocks)
- Prime the tubing to remove air bubbles
- Program your basal rates as prescribed by your doctor
- Calculate and deliver bolus doses for meals and high blood sugar corrections
- Monitor your blood glucose regularly to ensure proper function
- Change your infusion site every 2-3 days to prevent complications
For people living with diabetes who are tired of multiple daily injections, insulin pump therapy can bring welcomed relief. These small computerized devices deliver insulin continuously under your skin, mimicking how a healthy pancreas works.
Instead of taking several injections throughout the day, a pump provides a steady stream of insulin (basal) plus extra doses (bolus) when you eat or need to correct high blood sugar. About 350,000 people in the United States use insulin pumps, with approximately 90% having type 1 diabetes and 10% having type 2 diabetes.
Insulin pumps are not a cure for diabetes. They're tools that can make management easier when used correctly. Modern pumps have become more sophisticated, with some integrating with continuous glucose monitors (CGMs) to automatically adjust insulin delivery based on your real-time glucose levels.

What Is an Insulin Pump and How Does It Work?
An insulin pump is a small, computerized device that delivers rapid-acting insulin through a thin plastic tube (cannula) inserted under your skin. This continuous subcutaneous insulin infusion (CSII) mimics how a healthy pancreas functions.
Your pump works in two important ways:
Basal insulin flows continuously in small amounts throughout your day and night, keeping your blood glucose steady between meals and while you sleep.
Bolus insulin gives you extra doses when needed—like when eating or correcting high blood sugar readings.
One major advantage of how to use insulin pump therapy is that you'll only need rapid-acting insulin (like Humalog, NovoLog, or Apidra), offering more precise dosing compared to juggling both long-acting and rapid-acting insulins with injections.
Modern pumps often communicate wirelessly with continuous glucose monitors (CGMs), creating sensor-augmented systems. Some advanced models can even adjust your basal insulin automatically based on CGM readings. Learn more about pump benefits at MedlinePlus.
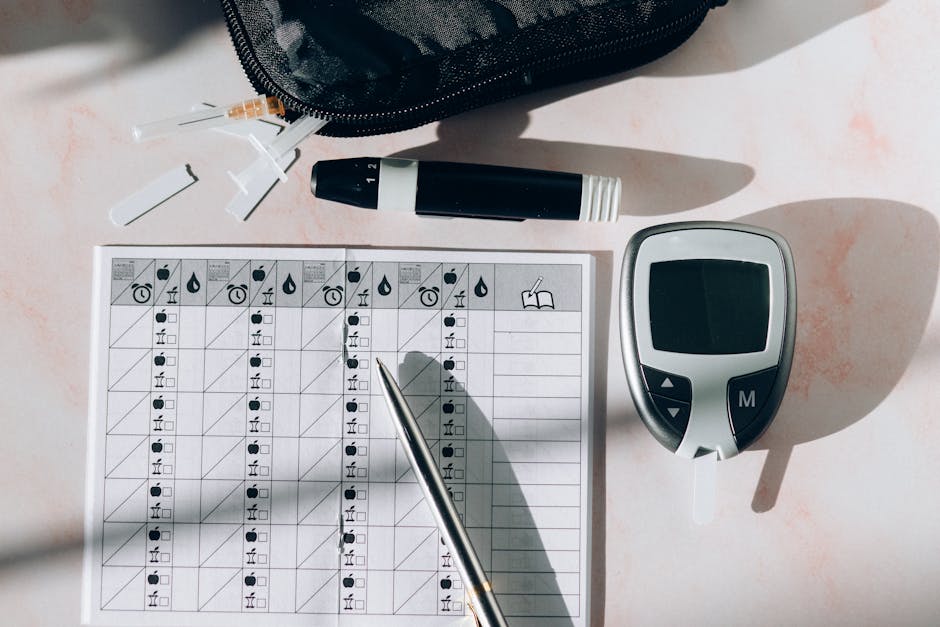
Key Components You'll Handle Daily
Living with a pump means becoming familiar with essential parts:
The insulin reservoir holds your insulin supply—typically enough for 2-3 days.
Your infusion set consists of thin, flexible tubing connecting the pump to the cannula. Change this every 2-3 days.
The cannula is a small, flexible tube that sits under your skin, usually in fatty tissue like your abdomen, buttocks, or thigh.
You'll use the pump controller to program insulin delivery, set basal rates, deliver bolus doses, and manage settings.
Pump Types at a Glance
Tubed Pumps connect to your body via thin tubing and can be temporarily disconnected when needed. Popular options include the Medtronic MiniMed series and Tandem t:slim.
Tubeless (Patch) Pumps eliminate visible tubing. These waterproof systems consist of a pod containing insulin that adheres directly to your body, controlled by a separate handheld device. The Omnipod system is a well-known example.
Hybrid Closed-Loop Systems integrate with CGMs to automatically adjust your basal insulin. Examples include Tandem Control-IQ and Medtronic MiniMed 780G.
| Pump Type | Pros | Cons | Best For |
|---|---|---|---|
| Tubed | More basal options, larger insulin capacity | Visible tubing, must disconnect for water activities | Tech-savvy users who want precise control |
| Tubeless | No tubing, waterproof, discreet | Limited basal options, smaller insulin capacity | Active individuals, those who want discretion |
| Hybrid Closed-Loop | Automated adjustments, less user intervention | More expensive, requires CGM | Those wanting the most automated experience |
At ProMed DME, we understand that choosing the right pump is a personal decision. Our dedicated diabetes care team can help you steer the options and assist with insurance coverage questions.
Who Can Benefit From Pump Therapy?
Wondering if an insulin pump is right for you? While these devices can be life-changing for many people with diabetes, they're not a one-size-fits-all solution.
Pump therapy is particularly beneficial for:- People with type 1 diabetes seeking more flexibility- Those with insulin-dependent type 2 diabetes tired of multiple daily injections- Pregnant women needing precise glucose control- Children and teenagers who appreciate fewer needle sticks- Active people with varying exercise routines
Pumps can also help those experiencing frequent low blood sugars, dawn phenomenon (high morning readings), or gastroparesis who benefit from extended bolus features.
According to the T1D Exchange registry, more than 60% of people with type 1 diabetes now choose pumps over multiple daily injections.
Cost is a consideration—an insulin pump can run as high as $6,500, with annual supplies adding another $2,000-$3,000. At ProMed DME, we work with most insurance plans to help minimize out-of-pocket expenses.
Advantages vs. Disadvantages to Weigh
Advantages:- More precise insulin delivery—some pumps can deliver as little as 0.025 units- One needle insertion every 2-3 days instead of multiple daily injections- Improved A1C levels and greater flexibility around meals, sleep, and exercise- Better management of dawn phenomenon and high-fat meals- CGM integration and detailed data tracking
Disadvantages:- Learning curve—pumps require some tech-savviness- Risk of diabetic ketoacidosis (DKA) if pump failure goes undetected- Adjustment to wearing a device 24/7 and possible skin irritation- Regular maintenance and typically higher costs than injections- Need for frequent monitoring and backup supplies
Choosing a Pump That Fits Your Life
Consider these factors when selecting your pump:- Size and weight for comfort and discretion- Interface preference: buttons, touchscreens, or remote controls- Waterproof ratings for swimming and water activities- Insulin capacity based on your typical usage- CGM compatibility with your preferred system- Battery type (rechargeable vs. replaceable)- Data sharing capabilities and alarm options- Quality of customer support and training
At ProMed DME, our dedicated nurse can help you steer these choices to find the pump that fits your lifestyle.
Research shows that success with pump therapy often depends more on the user's commitment than technical skills or diabetes type. The best candidates are those motivated to learn and actively participate in their care.
How to Use Insulin Pump Therapy – Step-by-Step Startup Guide

Starting insulin pump therapy begins with obtaining a prescription from your doctor. At ProMed DME, we help steer insurance approvals to maximize your benefits.
Proper training is essential before starting pump therapy. You'll work with a certified diabetes educator who will teach you everything from basic operation to troubleshooting. Many people practice with saline solution before switching to insulin.
Getting your supplies organized is crucial. You'll need your pump, insertion device, infusion sets, reservoirs, rapid-acting insulin, skin prep supplies, and backup supplies including syringes or pens with long-acting insulin for emergencies.
Your healthcare team will help determine your personal settings – basal rates, insulin-to-carb ratios, correction factors, target ranges, and active insulin time. These settings are the foundation of successful pump therapy.
For your first infusion set, cleanliness is key. Wash hands thoroughly and choose a site with fatty tissue – common spots include your abdomen, thighs, buttocks, or the back of your arms. After cleaning the area with alcohol and letting it dry, you're ready for insertion.
When filling the reservoir and priming tubing, remember: never prime the infusion set while it's connected to your body. Remove all air bubbles before connecting.
The insertion device makes placement quick and nearly painless. Once in place, secure with additional adhesive if needed and properly dispose of the insertion needle.

Programming Basal Rates & Bolus Doses
Your basal insulin covers your body's background needs – the insulin required even when not eating. Most people need different amounts at different times of day.
Finding your perfect basal rates takes testing. Your healthcare team will provide starting rates, then you'll test each time segment by fasting for several hours and checking glucose frequently. If levels stay steady (within about 30 mg/dL), you've found the right rate.
For meal boluses, enter your carbs and your pump calculates insulin needed based on your ratio. If you're at 1:10, that means 1 unit of insulin covers 10 grams of carbs.
Correction boluses help bring high readings back to target. Your correction factor tells the pump how much one unit of insulin lowers your blood sugar. Your pump tracks "insulin on board" to prevent dangerous stacking of insulin.
Modern pumps offer helpful advanced features like extended bolus (delivers insulin over several hours) and dual wave options (gives part immediately and the rest over time).
Daily Tasks & Responsibilities
Living with a pump means incorporating key habits into your routine:
- Regular blood glucose checks – at least 4 times daily if not using CGM
- Accurate carb counting for precise insulin dosing
- Changing infusion sets and reservoirs every 2-3 days
- Responding to pump alerts and alarms
- Reviewing pump data to spot trends
- Carrying backup supplies
Monitoring & Responding to Glucose Levels
Many modern pumps pair with continuous glucose monitoring (CGM) systems, providing real-time readings every few minutes. These systems show trend arrows indicating whether glucose is rising, falling, or stable.
For low blood sugar (below 70 mg/dL), follow the 15-15 rule: take 15 grams of fast-acting carbohydrate, wait 15 minutes, and recheck. For severe lows, you might temporarily suspend insulin delivery.
For high blood sugar, check your pump and infusion site for problems. Consider a correction bolus, stay hydrated, and check for ketones if above 250 mg/dL.
Ketone checking is crucial when blood sugar is unexpectedly high, you're feeling ill, or your pump has been disconnected for more than an hour. If ketones are present, change your infusion set immediately, take a correction dose with an insulin pen or syringe, drink plenty of water, and contact your healthcare provider if ketones are moderate or large.
Learning how to use insulin pump therapy takes time. At ProMed DME, our dedicated nurse is always available to provide support as you steer this journey.
Living Safely With Your Pump
Life with an insulin pump requires some planning, especially when traveling. Always pack twice the supplies you think you'll need and keep all diabetes supplies in your carry-on luggage—never check them.
Before crossing time zones, consult your healthcare provider about gradually adjusting basal rates. Your body doesn't immediately switch to a new time zone, and neither should your insulin delivery.
Airport security is manageable with insulin pumps. Most modern pumps are safe for standard security scanners, but check your manufacturer's guidelines. A simple "I'm wearing an insulin pump for diabetes" helps TSA agents know what to expect.
Exercise and your pump work well together with proper adjustments. Most people reduce basal rates by 50-80% during workouts using the temporary basal feature. For swimming or contact sports, you can disconnect for up to 60-90 minutes, checking glucose before, during (if possible), and after reconnecting.
Preventing diabetic ketoacidosis (DKA) requires vigilance when pump-dependent. Regular blood glucose checks help catch problems early. When you see unexplained high readings (above 250 mg/dL), check your tubing for kinks, your site for issues, and test for ketones if glucose remains liftd after correction.
Your backup supply kit should include:- Rapid and long-acting insulin- Syringes or pen needles- Blood glucose meter and test strips- Ketone testing supplies- Fast-acting glucose for treating lows- Extra pump supplies- Emergency contact information
Troubleshooting Common Issues
Occlusions occur when insulin can't flow properly through your infusion set. If you notice unexplained high glucose or an occlusion alarm, check for visible issues like kinked tubing and plan to change your infusion set. Give a correction dose with a pen or syringe while preparing your new set.
Air bubbles in tubing can affect insulin delivery. Let insulin reach room temperature before filling your reservoir, tap to move bubbles to the top, and prime thoroughly. If bubbles appear later, disconnect, re-prime to push them out, then reconnect.
Site infections or irritation need prompt attention. Watch for redness, warmth, swelling, pain, or rash. If these occur, remove the infusion set immediately, clean with antiseptic, and insert a new set elsewhere. Contact your healthcare provider if symptoms worsen.
For error messages or alarms, consult your user manual for specific troubleshooting steps. The manufacturer's support line can help with persistent issues. Consider reporting serious problems to the FDA's MedWatch program.
Caring for Your Pump & Skin
Clean your pump's exterior with a slightly damp cloth (never submerge unless waterproof). Monitor battery levels, keep buttons and screens debris-free, and follow guidelines for software updates.
Site rotation is crucial for effective insulin delivery. Develop a systematic pattern and allow sites to rest for 2-3 weeks before reusing them to prevent lipohypertrophy—fatty lumps that can develop from overused sites.
For adhesive reactions, try barrier films like Skin-Prep, experiment with different adhesive products, and remove adhesives slowly using proper removers or baby oil.
Weather and temperature affect both pump and insulin. Keep insulin between 36°F and 86°F, using insulated cases in hot weather and keeping your pump close to your body in cold weather.
Frequently Asked Questions About How to Use Insulin Pump Therapy
How often should I change my infusion set?
Change your infusion set every 2-3 days for optimal health and insulin absorption. Leaving it in longer can cause inflammation around the site, reducing insulin effectiveness and increasing infection risk.
The telltale sign you've waited too long? Unexplained high blood sugars that don't respond to correction boluses.
Different insulins have specific timelines: Humalog or NovoLog can remain in your pump reservoir for up to 6 days, while Apidra users should change every 2 days. Always follow your healthcare team's guidance and manufacturer recommendations.
What do I do if my pump alarms in the middle of the night?
When facing a middle-of-the-night alarm, check the message on your screen to determine the appropriate response:
- Occlusion alarms require changing your infusion set
- Low reservoir warnings can usually wait until morning if you have enough insulin to last
- Battery alerts need charging or replacement
- CGM connection issues may require checking sensor placement
Pro tip: Keep a diabetes "night kit" by your bed with essentials like spare infusion sets, backup insulin, glucose tablets, and a flashlight so you're prepared for any situation.
Can I switch back to injections temporarily?
Absolutely! There are many valid reasons for a pump break: device issues, extended swimming beyond waterproof capabilities, contact sports, or giving skin a rest from adhesives.
For short breaks (less than 12 hours), simply take rapid-acting insulin via injection to cover meals and corrections.
For longer breaks (more than 12 hours), you'll need to replace your basal insulin too. This means taking rapid-acting insulin for meals and corrections, plus adding long-acting insulin to replicate your pump's basal delivery. Your healthcare provider can help calculate the right long-acting dose based on your typical daily basal total.
Having a plan before you need it is key. At ProMed DME, we ensure our customers have access to both pump supplies and injection supplies, because flexibility is an important part of successful diabetes management.
Conclusión
How to use insulin pump therapy is a journey that combines education, practice, and daily attention to detail. While there's a learning curve initially, many patients find that once comfortable with their pump, the benefits transform their diabetes management experience.
Pump therapy requires active management through glucose monitoring, carb counting, regular infusion set changes, and troubleshooting occasional challenges. However, research consistently shows that people committed to long-term insulin pump therapy maintain better blood sugar control compared to those using multiple daily injections, leading to fewer complications and improved quality of life.
At ProMed DME, we understand that starting or optimizing pump therapy can feel overwhelming. That's why our dedicated nurse is always ready to answer questions and guide you through transitions or troubleshooting. We believe proper support makes all the difference in your success.
We offer a comprehensive range of diabetes supplies with free shipping nationwide and work with most insurance plans to keep out-of-pocket expenses low. Whether you're beginning your pump journey or fine-tuning current therapy, our team is here to help you achieve optimal diabetes management.
The technology behind insulin pumps continues to advance, making diabetes management increasingly precise and convenient. By partnering with us, you'll access both cutting-edge supplies and the human support that makes using them successfully possible.
For more information about our diabetes supplies and personalized support services, please visit our diabetes supplies section or reach out to our friendly team directly. We're looking forward to becoming a trusted part of your healthcare journey!
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.




