Skin-Friendly Pumping: Tips to Stop Insulin Pump Irritation

Skin-Friendly Pumping: Why Preventing Irritation Matters
If you use an insulin pump for diabetes, insulin pump skin irritation is a common and frustrating challenge.
Here are simple steps to help prevent it:
- Rotate your device sites often.
- Clean your skin well before application.
- Use skin barriers to protect your skin.
- Remove devices gently with adhesive removers.
Wearable diabetes technology like insulin pumps has revolutionized diabetes management, offering freedom and better blood sugar control. However, skin issues from device insertion and adhesives are a growing concern.
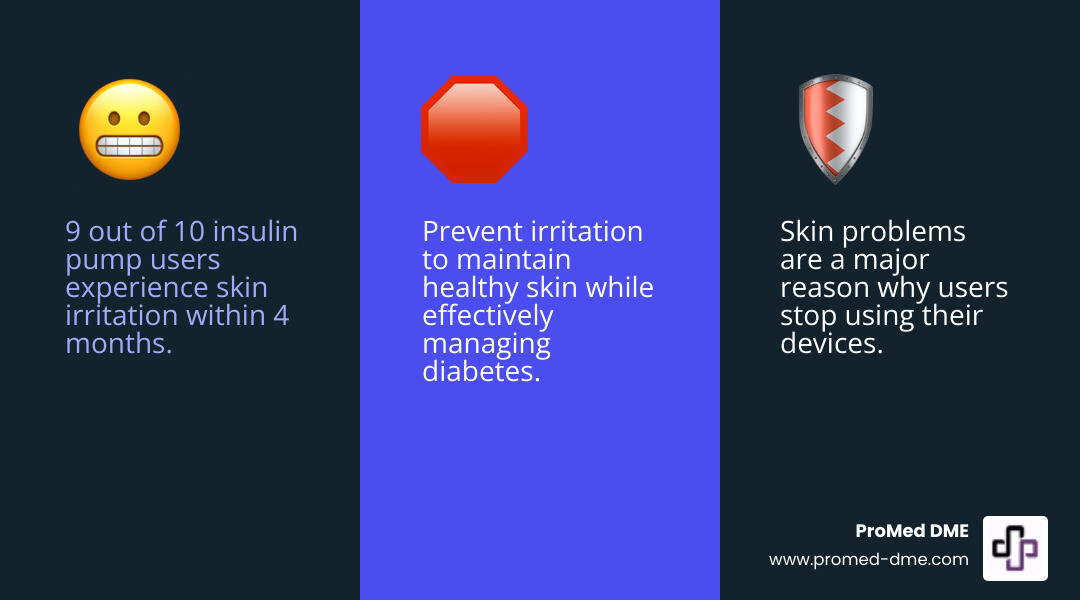
Within four months of use, 9 out of 10 people experience skin trouble like itching, redness, or wounds. These issues are a major reason people stop using their devices. But you don't have to choose between managing diabetes and healthy skin.
This guide explains why irritation happens and how to prevent it, offering clear steps and product tips to keep your skin healthy.
Essential Insulin pump skin irritation terms:
Understanding Skin Reactions from Diabetes Devices
While insulin pumps and continuous glucose monitors (CGMs) are incredible tools, they often cause skin issues. About 75% of users experience moderate itchiness, 66% redness, and 50% eczema. Half of pump users develop skin wounds, and 94% experience scarring. Unsurprisingly, nearly 20% of CGM users stop due to skin irritation.
Skin reactions generally fall into a few main types:
- Irritant Contact Dermatitis (ICD): The most common reaction (80% of cases), ICD is a non-allergic inflammation caused by direct skin damage. It's like a chemical burn or friction rash from adhesives, trapped moisture, or device pressure.
- Allergic Contact Dermatitis (ACD): Accounting for 20% of cases, ACD is a delayed allergic reaction. The immune system overreacts to an allergen in the device or adhesive, causing an itchy, red rash even with minimal contact.
- Mechanical Injury: Skin can tear during application or if adhesive is removed improperly. Pressure marks or damage can also occur if the sensor or cannula is too tight.
- Trapped Moisture: Sweat or water trapped under the device creates a moist environment ideal for bacterial growth and skin maceration (softening), leading to irritation and infection risk.
For a deeper dive into how our skin responds to these devices, you can explore Scientific research on skin integrity with device use.

Common Causes and Allergens
The main culprits for insulin pump skin irritation are often the complex chemical mixtures in device adhesives, which can cause sensitivities or allergies.
Common chemicals and allergens include:
- Acrylates: A family of chemicals common in medical adhesives known to be potent sensitizers.
- Isobornyl Acrylate (IBOA): A specific acrylate and significant allergen in some CGM adhesives. One study found 81% of patients with skin reactions to FreeStyle Libre were sensitized to IBOA.
- Colophonium (Rosin): A natural resin derived from pine trees that can cause allergic reactions.
- Cyanoacrylates: "Super glue" components that can be irritants or allergens.
Beyond adhesives, device components like plastic or cannula material can also trigger reactions in sensitive individuals. Manufacturers are working to develop less allergenic materials.
Are You at Higher Risk?
Anyone can experience insulin pump skin irritation, but certain factors increase your risk. Understanding them helps with proactive prevention:
- History of Atopic Dermatitis (Eczema): A history of eczema makes your skin more sensitive. These individuals are 30 times more likely to have skin problems with diabetes devices.
- General Sensitive Skin: If your skin reacts easily to products or fragrances, you're more susceptible to adhesive irritation.
- Female Gender: Contact dermatitis affects women twice as often as men, possibly due to hormones or higher exposure to chemicals in personal care products.
- Younger Age: Contact dermatitis often appears between ages 12-16. Since Type 1 Diabetes is common in those under 20, many young device users are at higher risk.
- Humid Climates and Excessive Sweating: Trapped moisture from humidity or sweat can lead to skin maceration and irritation. Athletes often face this challenge.
A Step-by-Step Guide to Preventing Insulin Pump Skin Irritation
Preventing insulin pump skin irritation is simpler than treating it. Success depends on three key steps: proper skin preparation, smart site placement, and gentle device removal.
Before You Apply Your Device
Proper skin preparation is crucial for good adhesion and less irritation.
Always start with clean skin. Wash the area with antimicrobial soap and water, or use an alcohol wipe to remove oils and dirt that can interfere with the adhesive.
Ensure the skin is completely dry. Let it air dry; don't blow on it. Avoid lotions and oils on the area, as they prevent proper adhesion and can trap moisture.
Let alcohol prep dry completely to avoid stinging and ensure good adhesion. If the site is hairy, trim or shave it 24 hours beforehand to prevent razor burn and improve adhesion, making removal easier.
Using a skin barrier can be a game-changer. These films or sprays create a protective layer between your skin and the adhesive. Apply a thin layer and let it dry completely.
Proper Site Rotation and Placement
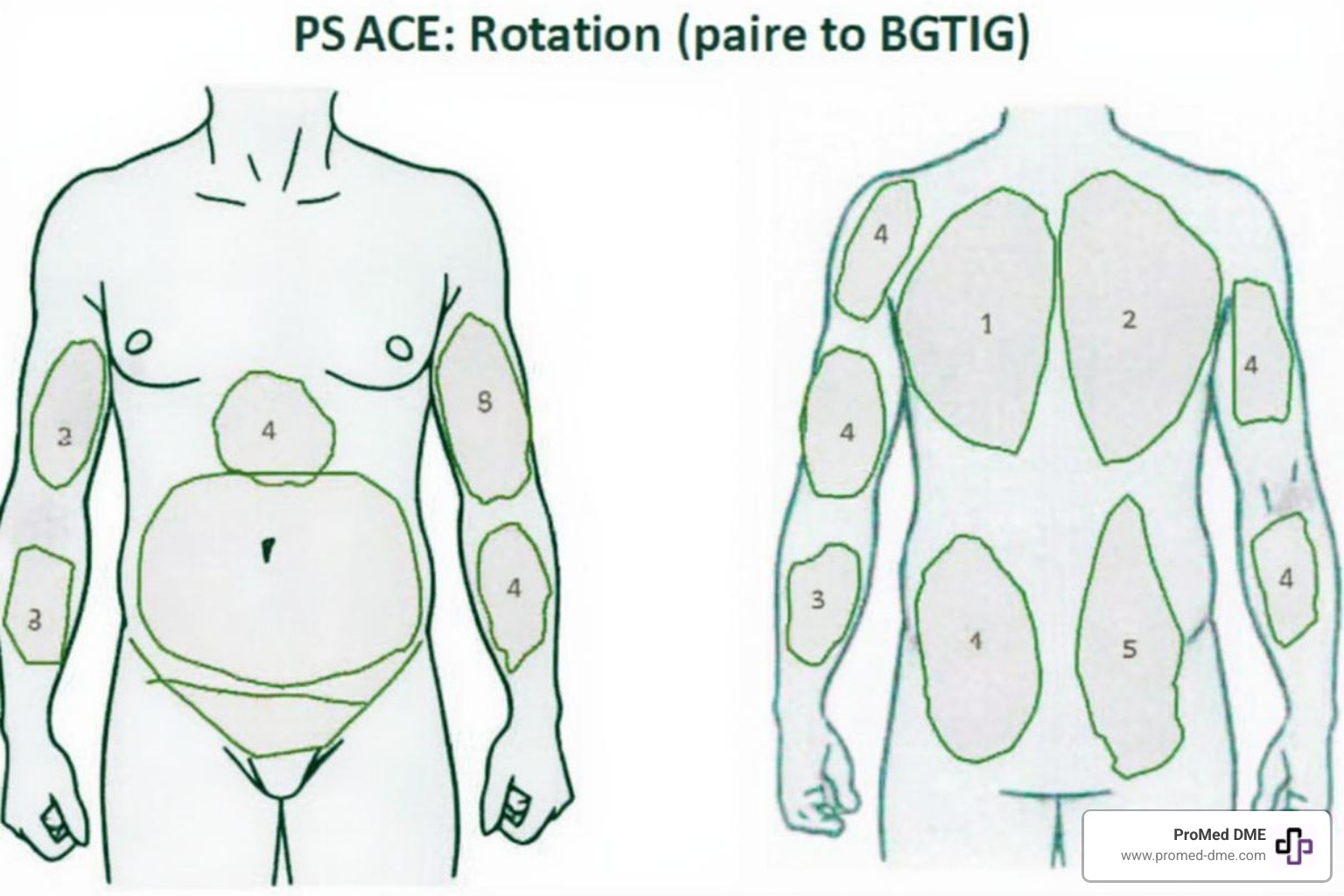
Regularly changing device sites is a golden rule. It prevents insulin pump skin irritation and also improves insulin absorption and glucose reading accuracy.
Change sites regularly: every 2-3 days for insulin pumps and 10-14 days for CGMs. Keep a site chart to ensure you rotate spots and allow old sites to heal, which is crucial if you wear both a pump and a CGM.
Avoid scarred tissue and lipodystrophy areas (lumps or dents from repeated insertions). These areas absorb insulin unreliably and are prone to irritation. Give sites a rest by allowing at least 10 days for a spot to recover before reusing it.
Here are some tips for strategic placement:
- Choose a new site at least one inch away from the last one.
- Avoid placing devices over moles, tattoos, scars, or stretch marks.
- Keep devices at least two inches away from your belly button.
- Pick flat areas that won't rub against clothes.
- Never put a device on skin that has an active infection or irritation.
- If wearing multiple devices, ensure they are far enough apart and check instructions for wireless communication needs.
For more detailed guidance, check out these Tips for infusion set best practices.
The Right Way to Remove Your Device
Gentle removal is as important as proper application. Ripping off an adhesive can strip skin layers, causing insulin pump skin irritation, pain, and wounds.
Use an adhesive remover like Detachol™, Tac Away™, or Uni-solve™ to loosen medical adhesives. In a pinch, baby or olive oil can work. Apply the remover to the adhesive's edge and let it soak in.
First, gently loosen the edges. Then, peel low and slow, pulling the adhesive parallel to your skin, not straight up (the "fold back" technique). Alternatively, use the "stretch and relax" technique by stretching the adhesive horizontally while sliding your fingers underneath.
After removal, cleanse the skin with warm, soapy water to remove residue. Rinse well and gently pat dry.
Your Toolkit: Essential Products for Healthy Skin
Managing insulin pump skin irritation is easier with the right products. Finding what works for your skin may take some trial and error, but it can make all the difference.
Barrier Films and Sprays create a breathable shield between your skin and the adhesive, preventing irritation and improving adhesion. Popular options include Cavilon™ by 3M, Skin-Prep™ by Smith and Nephew, and AllKare® by Convatec. Let them dry completely before applying your device.
Hydrocolloid Dressings like Tegaderm™ or IV3000™ can be cut to fit under your device, offering a cushioned barrier. You can cut a hole for the cannula to pass through. For a custom fit, Underlay Patches are pre-cut for specific devices like Omnipod or Dexcom and go under the device's adhesive. Brands include Not Just a Patch, The Sugar Patch, Skin Grip, and ExpressionMed.
Adhesive Removers are essential for gentle device changes. Wipes or sprays like Detachol™ by Eloquest, Tac Away™ by Torbot, and UNI-SOLVE™ Adhesive Remover by Smith and Nephew loosen medical adhesives, preventing skin stripping and insulin pump skin irritation. In a pinch, household oils like baby or coconut oil can also work.
If you're active or live in a humid climate, Over-tapes for extra security can help keep your device in place. Options include Hypafix tape® by BSN Medical, Mefix tape® by Molnlycke health Care, and Tegaderm® by 3M. Nexcare Coban® is a self-adherent wrap, while Hy-Tape is great for sensitive skin. Decorative options like GrifGrips® are also available. A "picture frame" taping technique can also add reinforcement.
After removal, Soothing Post-Removal Creams can help. A gentle moisturizing lotion can soothe and protect tender skin. For mild redness or itching, an over-the-counter hydrocortisone cream can provide relief.
Natural Remedies for Skin Care
Beyond commercial products, many people find relief with natural remedies for irritated skin.
Coconut Oil has moisturizing and anti-inflammatory properties. Use it to remove adhesive residue or soothe dry skin. Castor Oil is also anti-inflammatory and promotes healing when applied topically. You can explore Scientific research on skin integrity with device use to learn more.
Jojoba Oil is an excellent moisturizer similar to the skin's natural oils. Rose Water has anti-inflammatory properties that can calm irritated skin. As mentioned, baby oil and olive oil can also be used as gentle adhesive removers and moisturizers.
Always perform a patch test before using natural remedies. For persistent or severe issues, consult your healthcare provider.
Managing and Treating Existing Skin Issues
Despite prevention efforts, insulin pump skin irritation can still occur. It's important to respond quickly to prevent a minor issue from becoming a serious infection or causing long-term skin damage.
How to Treat Mild Insulin Pump Skin Irritation
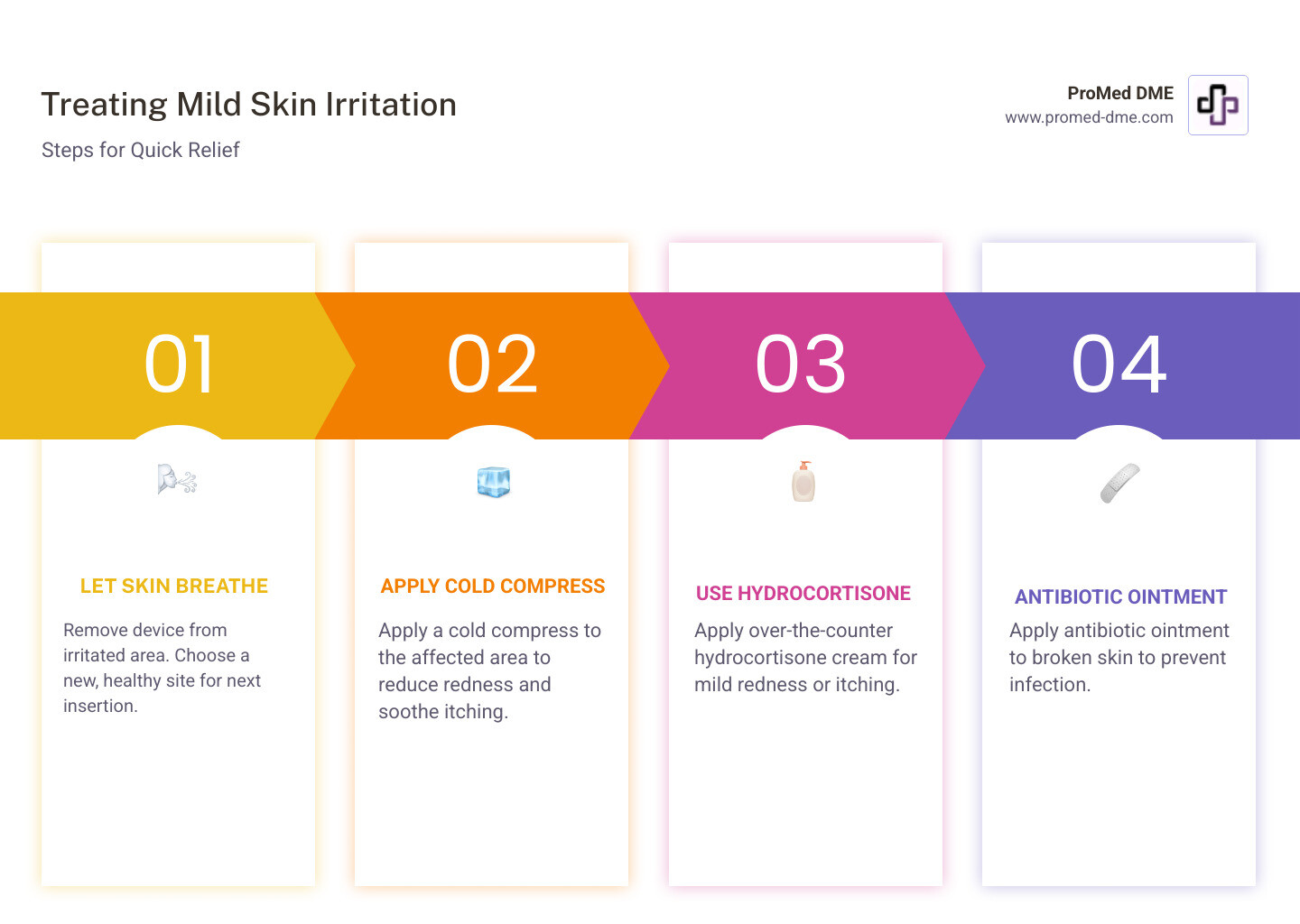
If you notice mild, non-spreading redness, itching, or a rash, here's how to help your skin heal:
- Let the skin breathe. Remove the device from the irritated spot immediately and choose a new, healthy site for your next insertion.
- Apply a cool compress. A clean, cool compress can provide immediate, soothing relief from itching and redness.
- Use hydrocortisone cream. For itchy, inflamed, but unbroken skin, a thin layer of over-the-counter 1% hydrocortisone cream can calm the irritation.
- Apply antibiotic ointment. If the skin is broken but not infected, apply an over-the-counter antibiotic ointment like Polysporin. For pain and itching on intact skin, some find relief by dabbing on a liquid antacid like Maalox. Always clean the area first.
- Cleanse the area. After removal, cleanse the skin with mild soap and water to remove adhesive residue. Pat dry gently.
Addressing Severe Insulin Pump Skin Irritation
More serious skin irritation requires professional attention. Watch for these red flags:
- Blisters
- Oozing wounds
- A spreading rash
Signs of infection require immediate medical attention. Look for:
- Increasing Redness: Especially if the red area is larger than 1 cm around the site.
- Tenderness or Increased Pain
- Pus or Pustules
- Warmth around the site
- Swelling
- Fever or Chills
- Lifted Blood Glucose Levels, which can be a sign of infection.
If you see any severe signs, call a healthcare professional immediately. Do not treat a suspected infection yourself. Change your site, clean the area, and seek medical advice to see if you need antibiotics or other treatment.
The Importance of Healthy Skin for Diabetes Management
Healthy skin is a vital partner in your diabetes journey. It's crucial for effective diabetes management, not just comfort. Unhealthy skin can disrupt blood glucose control, and chronic insulin pump skin irritation can lead to serious long-term consequences.
A major concern is lipodystrophy, or changes in fatty tissue, which appears in two forms:
- Lipohypertrophy: Repeated insertions in the same spot cause lumps of hardened fat. Insulin absorption in these areas is unpredictable, leading to erratic blood sugar levels. Studies confirm how lipohypertrophy impairs insulin absorption. Learn more here: How lipodystrophy can affect insulin absorption.
- Lipoatrophy: Less common today, this is the loss of fatty tissue, creating dents in the skin. Like lipohypertrophy, it also impairs insulin absorption.
Scarring is also a significant issue for many pump users. Scars can act like roadblocks, preventing consistent insulin absorption, similar to lipodystrophy.
Damaged skin from lipodystrophy, scarring, or inflammation absorbs insulin unpredictably, leading to unexplained high blood sugars. For CGM users, inflammation or pressure can cause falsely low readings (Pressure Induced Sensor Attenuation or PISA), often from lying on the sensor.
Skin issues are a leading reason people stop using pumps or CGMs. No one should have to choose between advanced diabetes management and healthy skin.
When to Consult a Healthcare Professional
While many issues can be handled at home, it's important to know when to call a professional. Seek medical advice for any of the following:
- Persistent Irritation: Redness, itching, or discomfort that doesn't resolve within 24 hours with home treatment.
- Worsening Symptoms: Irritation that is spreading, worsening, or becoming more painful.
- Suspected Infection: Signs like increasing redness (>1 cm), pus, warmth, fever, or unexplained high blood glucose require prompt medical attention.
- Suspected Allergic Contact Dermatitis (ACD): Intense itching, blistering, or a distinct rash pattern may indicate an allergy that needs professional diagnosis.
- Need for Patch Testing: For severe, recurring reactions, a dermatologist can perform patch testing to identify a specific chemical allergen.
- Consulting a Dermatologist: A dermatologist can provide specialized treatment for chronic or severe skin problems related to your devices.
- Speaking with a Diabetes Educator: A diabetes educator is a great resource for troubleshooting skin issues. They can review your techniques and suggest products.
At ProMed DME, we truly believe that managing diabetes is a team effort. That's why we have a dedicated nurse on staff who understands these challenges and is ready to provide guidance. Please don't hesitate to reach out to us with your questions and concerns.
Conclusión
Using insulin pumps and CGMs while keeping your skin healthy is a balancing act, but it's a manageable challenge. This guide has covered why insulin pump skin irritation occurs, who is at risk, and how to prevent and treat it.
Prevention is your best strategy. This includes meticulous skin preparation, diligent site rotation to ensure proper insulin absorption, and gentle device removal. A well-stocked toolkit of skin products is essential. Knowing how to manage mild issues and when to seek professional help from your healthcare team is also critical.
You don't have to choose between effective diabetes management and healthy skin. Being proactive reduces discomfort, improves device performance, and boosts your quality of life.
At ProMed DME, we get it. We understand the daily realities of living with diabetes, and our commitment goes far beyond just providing your supplies. We’re proud to have a dedicated nurse on staff who is knowledgeable about these common skin challenges and can offer guidance. We also work with most insurance plans to help minimize your out-of-pocket expenses and offer free shipping across the United States. Our goal is simple: to make sure you have top-quality products and exceptional customer service, supporting you every step of the way on your diabetes management journey.
Find your diabetes care supplies today
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.