Pump Up Your Diabetes Management with Sensor-Augmented Insulin Pumps
Simplified Diabetes Management: An Introduction
Living with diabetes often involves constant attention to blood sugar levels and insulin doses. But a insulin pump with sensor system can truly simplify this process. These smart devices work together to provide automated insulin delivery, helping you manage your diabetes with greater ease and confidence.
Here's a quick look at what an insulin pump with a sensor offers:
- What it is: It’s a small device that delivers insulin, paired with a continuous glucose monitor (CGM) that constantly tracks your blood sugar levels.
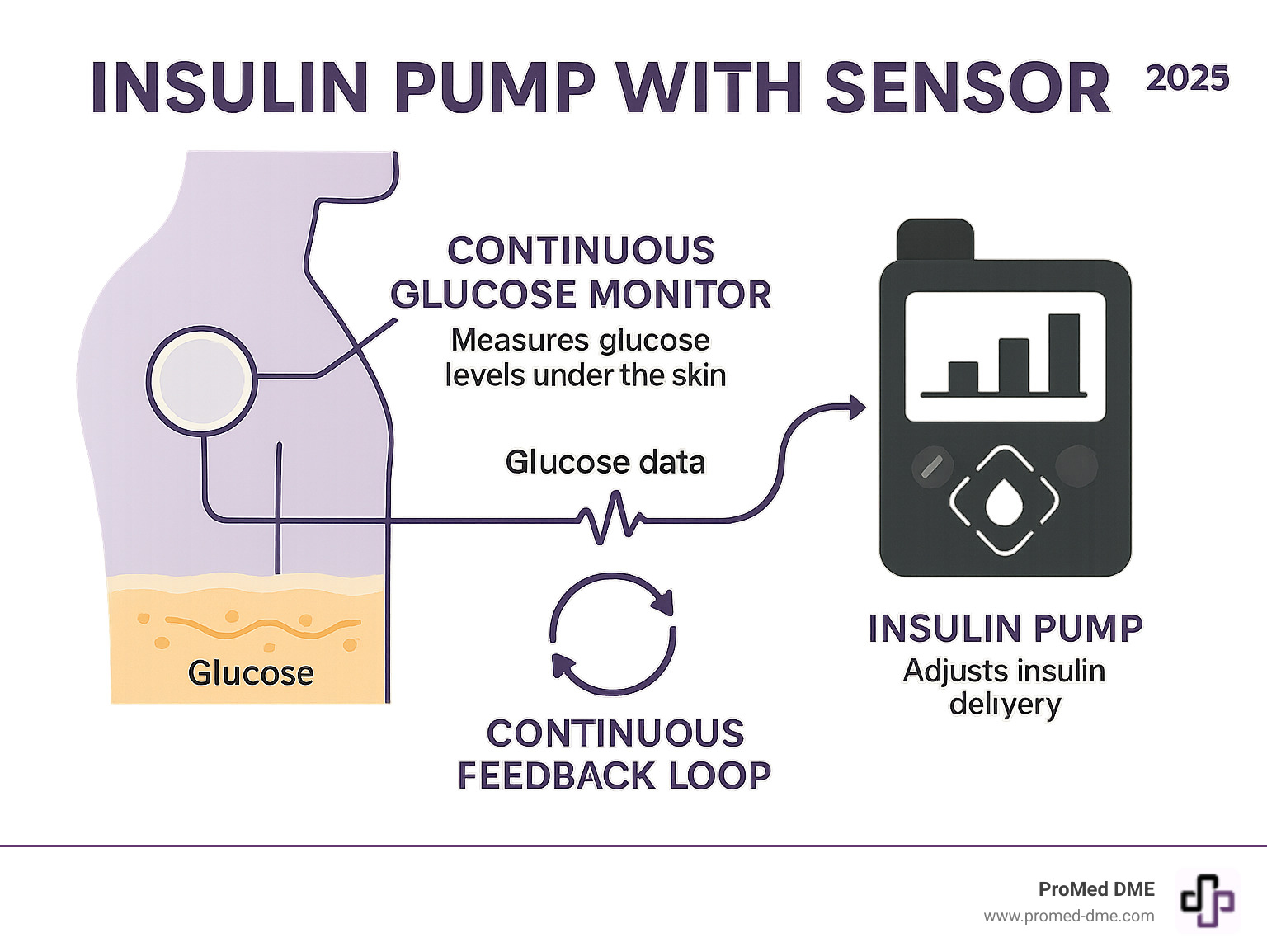
- How it works: The sensor sends real-time glucose data to the pump, which then automatically adjusts insulin delivery. This mimics how a healthy pancreas works.
- How it helps: This integration can reduce the burden of frequent manual checks and injections, giving you more freedom and peace of mind. As one user shared, "Using an insulin pump system made my life with diabetes so much easier."
This guide will explain how these advanced systems work, their many benefits, and how they can empower you to live your life to the fullest.
Important Insulin pump with sensor terms:
The Two Pillars of Modern Diabetes Tech: Insulin Pumps and CGMs
To truly understand how an insulin pump with sensor system revolutionizes diabetes management, first grasp the role of each component individually. These two technologies, when combined, create a powerful synergy that simplifies daily care.
What is an Insulin Pump?
An insulin pump is a small, computerized device designed to deliver insulin continuously throughout the day, closely mimicking the way a healthy pancreas releases insulin. This method is often referred to as Continuous Subcutaneous Insulin Infusion (CSII). Unlike traditional multiple daily injections (MDI), which involve several discrete shots, a pump provides a steady, measured flow of insulin (known as the basal rate) 24 hours a day.
When it's time to eat, or if your blood glucose levels are high, you can instruct the pump to deliver an additional surge of insulin, called a bolus dose. This can be done quickly and discreetly, often by simply pressing a few buttons on the pump or a connected device.
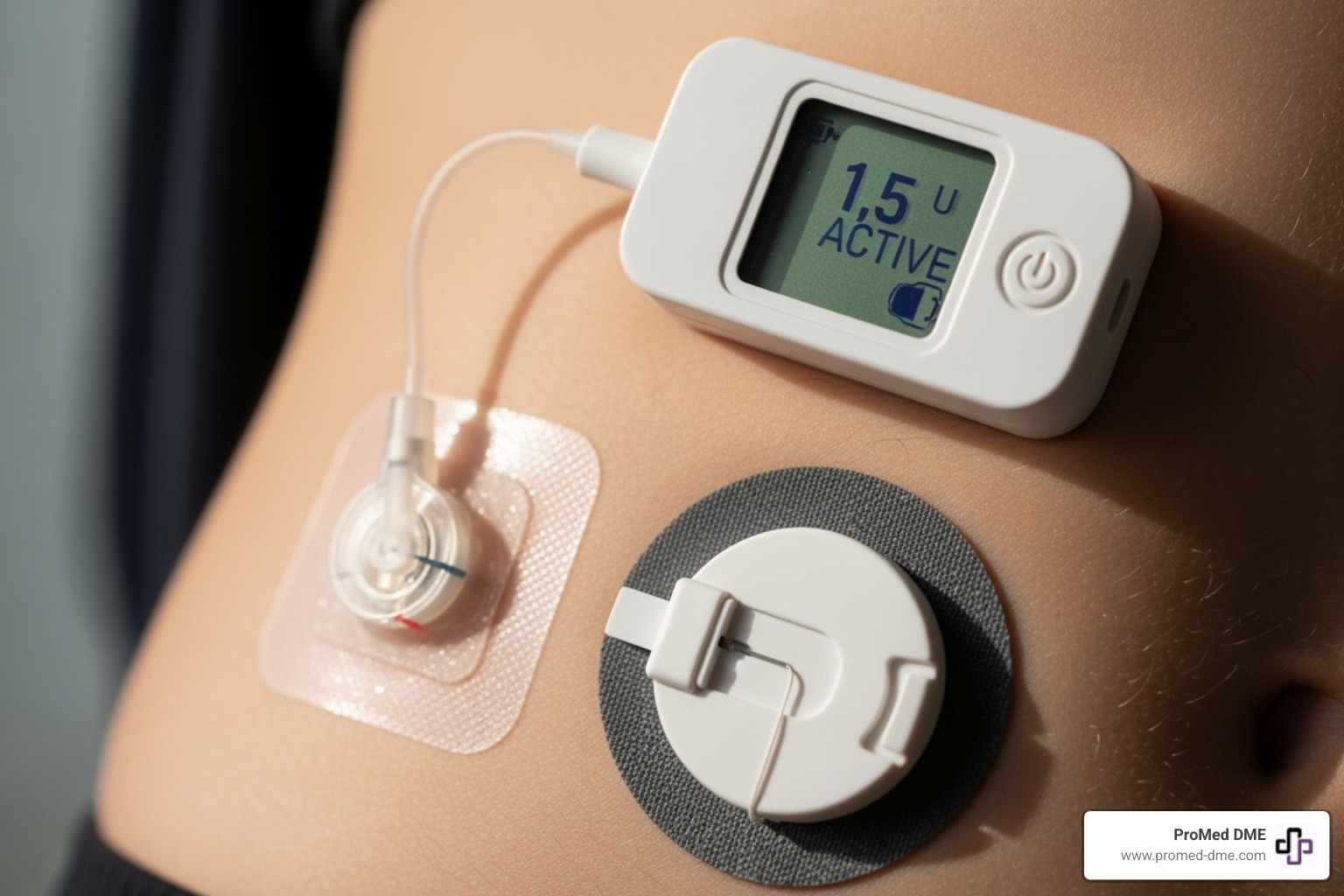
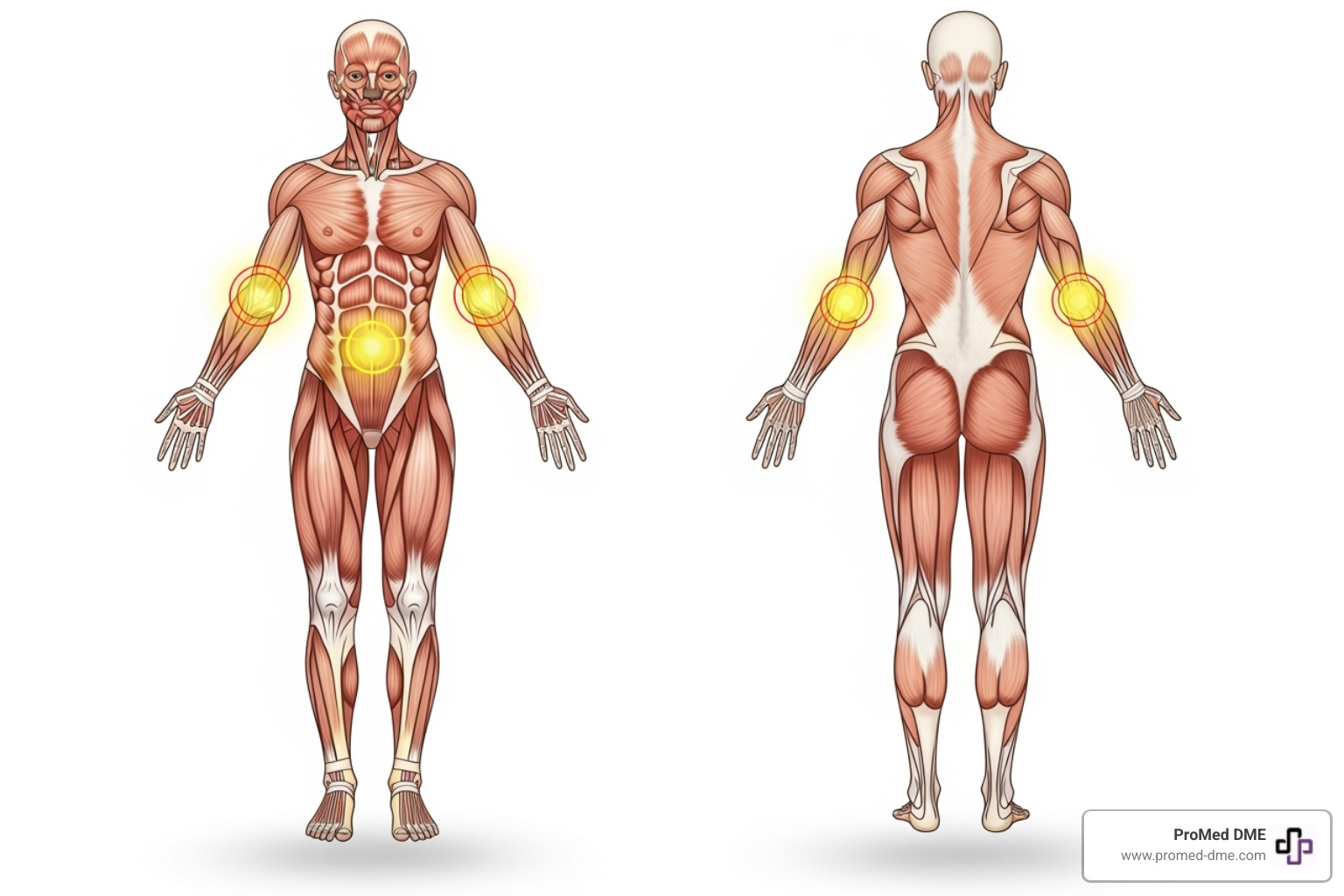
Insulin is infused into your fatty tissue through a thin, flexible plastic tube called a cannula, which is part of an infusion set. This set is inserted just under the skin, usually in the abdomen, thigh, or arm, and is typically changed every two to three days to prevent infection and ensure proper absorption. Only rapid-acting insulin is used in a pump. Over the decades, pumps have become significantly smaller, more user-friendly, and packed with advanced capabilities.

What is a Continuous Glucose Monitor (CGM)?
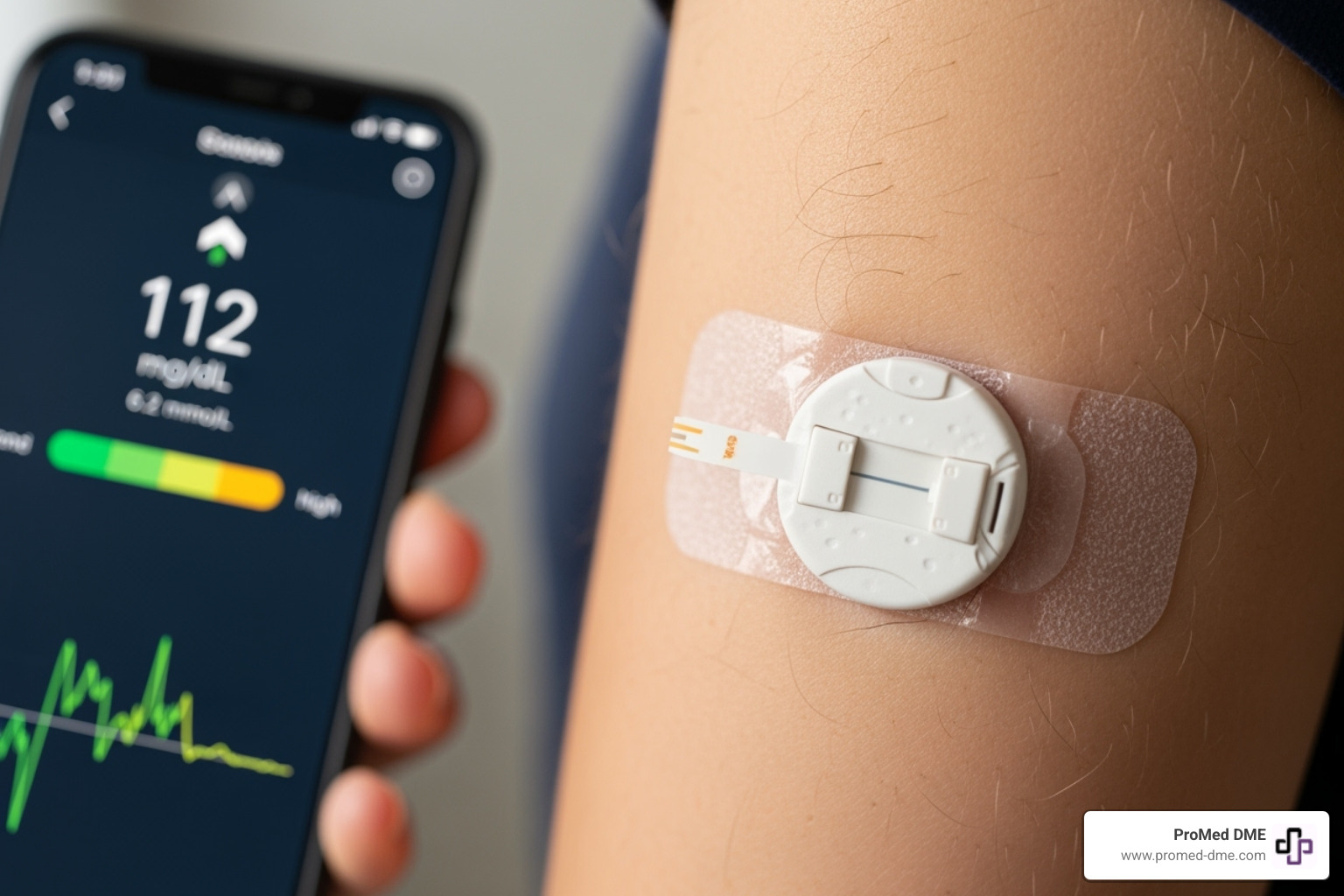
A Continuous Glucose Monitor (CGM) is a small, wearable device that tracks your glucose levels around the clock. It consists of a tiny sensor inserted just under the skin, which measures glucose in the interstitial fluid (the fluid surrounding your cells). This sensor is connected to a small transmitter that wirelessly sends glucose information to a receiver or a compatible smartphone.
Unlike traditional fingerstick blood glucose meters, which give you a single snapshot of your glucose at a specific moment, a CGM provides a continuous stream of data. You can see your current glucose level, a history of your levels, and, crucially, the direction your glucose is heading (e.g., rising, falling, stable). This real-time information allows you to anticipate and prevent both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar).
Many modern CGM systems are factory-calibrated, meaning they don't require daily fingerstick calibrations, making monitoring even easier. Some are even FDA-approved to replace daily blood glucose checks for treatment decisions. CGMs offer invaluable insights, helping you understand how food, exercise, stress, and medication impact your glucose levels. They provide alerts when your glucose goes too high or too low, offering peace of mind and enabling proactive management.
The Synergy: How an Insulin Pump with Sensor Creates a Smart System
When you bring an insulin pump and a CGM together, something remarkable happens. These two devices don't just work side by side – they actually communicate with each other through Bluetooth technology, creating what's called a sensor-augmented pump (SAP). Think of it like giving your insulin pump eyes to see what's happening with your blood sugar.
But the real excitement comes with Automated Insulin Delivery (AID) systems. These represent the next level, where smart algorithms and predictive technology work behind the scenes to make automatic adjustments. It's like having a tiny pancreas that never sleeps, constantly working to keep your glucose levels stable.
How Sensor-Augmented Pumps (SAP) Work
With a sensor-augmented pump, your insulin pump with sensor becomes much smarter. The CGM sends real-time glucose readings directly to your pump's screen, so you always know where your levels stand without pulling out a separate device.
The beauty of this setup lies in features like low glucose suspend and predictive low-glucose suspend. When your CGM detects that your glucose is dropping or predicts it will drop soon, you can quickly pause insulin delivery with just a few button presses. This simple action can prevent a scary low blood sugar episode before it happens.
Many people find this reduces their fear of hypoglycemia significantly. Instead of constantly worrying about surprise lows, you get early warnings that let you take action. Studies show that people using SAP systems achieve better HbA1c levels without experiencing more low blood sugar episodes – a win-win situation.
The Leap to Automated Insulin Delivery (AID)
Here's where things get really exciting. Automated Insulin Delivery systems, often called hybrid closed-loop systems, take that communication between devices and add artificial intelligence to the mix. These systems don't just show you glucose data – they actually use it to make decisions.
The smart algorithms in these systems are constantly analyzing your glucose trends, predicting where your levels are heading, and making tiny adjustments to your basal insulin every few minutes. Some systems can even deliver small correction boluses automatically when they detect your glucose climbing too high.
This technology comes remarkably close to mimicking a healthy pancreas. Your natural pancreas constantly monitors glucose and releases just the right amount of insulin at just the right time. While we're not quite there yet with artificial systems, we're getting impressively close.
You'll still need user input for meals – the system needs to know when you're eating and approximately how many carbs you're consuming. That's why these are called "hybrid" systems. But between meals, during exercise, and while you sleep, the system works tirelessly to keep your glucose in a healthy range.
The scientific research on hybrid closed-loop systems continues to show promising results, with users experiencing better glucose control and improved quality of life. It's truly remarkable how far diabetes technology has come in recent years.
Opening up Better Control: The Benefits of Sensor-Augmented Pumping
Combining an insulin pump with a sensor isn't just about technology; it's about changing how you live with diabetes every day.
Key clinical benefits of an insulin pump with sensor
The numbers are impressive. People using an insulin pump with sensor typically spend about 76% of their time in the healthy glucose range (70-180 mg/dL). This represents hours of feeling better, thinking clearer, and worrying less.
- Improved glycemic control: Studies consistently show that pump therapy with CGM leads to lower HbA1c levels and better blood sugar control compared to multiple daily injections.
- Increased Time in Range: Staying in the target glucose zone more often is a key benefit that leads to better long-term health outcomes.
- Reduced risk of hypoglycemia: A major advantage is the system's ability to predict and prevent low blood sugar episodes, providing tremendous peace of mind. Research confirms that CGM use significantly reduces these events.
- Better sleep quality: With fewer overnight highs and lows to worry about, you can get the restorative rest your body needs.
Other clinical benefits include lower total daily insulin doses, fewer episodes of diabetic ketoacidosis (DKA), and even improved cognitive function in some older adults. For comprehensive research backing these benefits, you can explore the evidence on improved outcomes that researchers have documented.
How an insulin pump with sensor impacts daily life
The real magic is in the everyday moments, like a spontaneous dinner without needing an injection or a morning jog without fear of your blood sugar crashing.
- Greater flexibility: You're no longer tied to rigid injection schedules for meals and exercise. You can adjust insulin delivery on the spot.
- Freedom from multiple daily injections: No more carrying pens or syringes everywhere. The pump delivers insulin continuously and discreetly.
- Confidence with exercise: Real-time glucose data and the ability to adjust insulin delivery make physical activity less intimidating.
- Discretion: Modern pumps are small and easily hidden, allowing you to manage your diabetes without drawing attention.
- Peace of mind for caregivers: Remote monitoring capabilities allow trusted family members to view glucose trends and receive alerts.
As one user put it, the integration "took such a weight off my shoulders" by eliminating the constant "guessing game." When technology handles the minute-to-minute adjustments, you're free to focus on living your life. At ProMed DME, we've seen how these systems create a foundation for not just better diabetes management, but a more fulfilling life.
Navigating Your Journey: Is This Technology Right for You?
Deciding to use an insulin pump with sensor is a significant step. It's a personal choice that involves understanding the technology, your readiness for it, and practical considerations like cost and safety.
Who is a Good Candidate for Pump Therapy?
While not a one-size-fits-all solution, pump therapy offers immense benefits for many. You might be a good candidate if you:
- Have Type 1 Diabetes. Systems are approved for a wide range of ages, from young children (like with Omnipod 5) to adults (like with MiniMed™ 780G).
- Have Type 2 Diabetes and require intensive insulin therapy.
- Are currently on multiple daily injections (MDI) and want to simplify your routine.
- Are motivated for active management and willing to learn carbohydrate counting.
- Seek greater flexibility, improved glucose control, and reduced hypoglycemia.
- Maintain open communication with your healthcare team for training and ongoing support.
Potential Risks and Safety Considerations
While these systems offer great advantages, it's important to understand the potential risks. Responsible use is key.
- Infusion Site Issues: The most common problems are infections and skin irritation. Prevent them by changing your infusion set every 2-3 days (or up to 7 for extended-wear sets), practicing good hygiene, and rotating sites to let skin heal.
- Diabetic Ketoacidosis (DKA) Risk: An interruption in insulin delivery from a pump malfunction or dislodged set can lead to DKA. Always have backup insulin supplies (syringes/pens) available.
- Tubing Snags: For tubed pumps, the tubing can snag and pull out the infusion set.
- Alarm Fatigue: Too many alarms can lead to users ignoring them. Some systems have features to help reduce this.
- Medication Interference: Some medications (like hydroxyurea) can cause false CGM readings. Inform your doctor of all medications you take.
- Device Removal for Procedures: You must remove your pump and CGM before MRI, CT, or diathermy treatments.
- User Responsibility: Even with automation, you are an active participant. This includes testing blood glucose as recommended, accurately counting carbs for meals, maintaining self-care skills, and seeing your healthcare provider regularly.
Costs and Insurance Coverage
Understanding the costs and navigating insurance can seem daunting, but we're here to help.
- Device Costs: The pump is a durable medical equipment (DME) item, while sensors and supplies are covered under either your pharmacy benefit or DME.
- Out-of-Pocket Expenses: Your costs will vary depending on your insurance plan's deductible, co-pays, and co-insurance. Prior authorization is often required.
- Medicare Coverage: Systems like the MiniMed™ 780G and Omnipod 5 are covered by Medicare and Medicare Advantage for eligible individuals.
- Trial Programs: Some manufacturers offer trial or copay assistance programs.
- Our Commitment: At ProMed DME, we understand these complexities. Our team works with most insurance plans to help minimize your out-of-pocket expenses. We also offer free shipping across the United States, ensuring that getting your essential supplies is as convenient and affordable as possible. Our dedicated nurse on staff is also available to answer your questions and guide you through the process, making sure you have the support you need.
Frequently Asked Questions about Insulin Pumps with Sensors
It's normal to have questions when considering a new technology like an insulin pump with sensor system. Here are answers to some common queries.
What is the difference between a sensor-augmented pump and an automated insulin delivery system?
Think of it as two levels of technology.
A Sensor-Augmented Pump (SAP) shows real-time glucose data from your CGM directly on your pump. This allows you to see your levels and trends, but you still make the decisions, like bolusing for meals or suspending insulin for a predicted low. Some SAPs have a "low glucose suspend" feature to help prevent hypoglycemia.
An Automated Insulin Delivery (AID) System, or Hybrid Closed-Loop, is the next level. A smart algorithm uses CGM data to automatically adjust your background (basal) insulin 24/7. It can even give small correction doses for high glucose. You still need to bolus for meals, but the system handles much of the fine-tuning, reducing the mental load of diabetes management.
How often do I need to change my pump infusion site and CGM sensor?
Both parts of an insulin pump with sensor system are designed for multi-day wear, but the exact timing depends on the brand.
- Pump Infusion Site: Most standard sets should be changed every two to three days (48-72 hours) to prevent infection and ensure good insulin absorption. Some extended-wear sets can last up to 7 days.
- CGM Sensor: The lifespan varies by model. Many popular sensors are worn for 7 to 14 days (e.g., Dexcom G7 lasts 10 days). Some implantable sensors can last for 90 to 180 days.
Always follow the manufacturer's instructions for your specific devices.
Can I still swim, shower, and exercise with these devices?
Yes, absolutely! Modern insulin pump with sensor systems are designed for an active lifestyle.
Many pumps and CGM components are water-resistant or waterproof, allowing you to shower, bathe, and swim. Always check the specific water-resistance rating for your model, as limits vary. For some activities, you can temporarily disconnect a tubed pump from its infusion set (usually for no more than an hour). Tubeless patch pumps, like the Omnipod, offer great freedom for water activities without needing to disconnect.
For exercise, these systems are a game-changer. Real-time glucose data and the ability to set a temporary basal rate allow you to manage your blood sugar with much more confidence and control during physical activity. For personalized advice, always chat with your healthcare provider.
Conclusión
Wow, what a journey! We've seen how the insulin pump with sensor system has truly changed the game for diabetes management. It's not just about numbers on a screen; it's about giving you more freedom, greater control, and a whole lot more peace of mind. Imagine less worry about lows, more stable blood sugar, and simply more time to live your life to the fullest!
This amazing technology is all about empowering you. It helps make managing diabetes less of a burden and more of a natural part of your day. It’s like having a smart assistant constantly looking out for your health.
Here at ProMed DME, we get it. We believe everyone deserves the best tools and support for their diabetes journey. That's why we're dedicated to bringing you top-quality durable medical supplies. Our goal is to make getting your supplies as easy and stress-free as possible. We offer free shipping across the United States, and our friendly team works hard to sort out insurance complexities, helping to keep your out-of-pocket costs down. Plus, we even have a dedicated nurse on staff ready to answer your questions and offer guidance along the way. We're here for you!
Choosing an insulin pump with sensor is a big step towards a future where managing diabetes is simpler, more automated, and helps you feel healthier every day. We are truly here to help you thrive.
Ready to explore how an insulin pump with sensor can transform your diabetes management? The first step is always to chat with your healthcare provider. You can Schedule an Appointment with them to discuss if this technology is right for you. Once you've made that decision, our team at ProMed DME is ready to support you with all the supplies and care you need.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.



