Demystifying Blood Glucose Monitoring: Devices Explained

Why Monitoring Your Blood Glucose is Crucial
A blood glucose monitoring device measures the amount of sugar (glucose) in your blood and is arguably the most important tool in your diabetes management toolkit.
What you need to know about blood glucose monitoring devices:
- Traditional meters require a drop of blood from your finger for instant results.
- Continuous glucose monitors (CGMs) use a sensor under your skin to track glucose levels every few minutes.
- Both types help you make better decisions about food, exercise, and medication.
- Insurance coverage varies, but many devices are covered for people with diabetes.
- Accuracy matters - proper technique and maintenance ensure reliable readings.
Managing diabetes without monitoring your blood glucose is like driving blindfolded. The landmark Diabetes Control and Complications Trial proved that people with diabetes who used home monitors to maintain good glucose control had significantly fewer disease complications over time.
A diabetes diagnosis can feel overwhelming, but modern blood glucose monitoring devices have come a long way. They are easier to use, more accurate, and less painful than ever before.
Understanding your options is the first step toward taking control of your health. The right device becomes your partner in making informed decisions about your daily care.
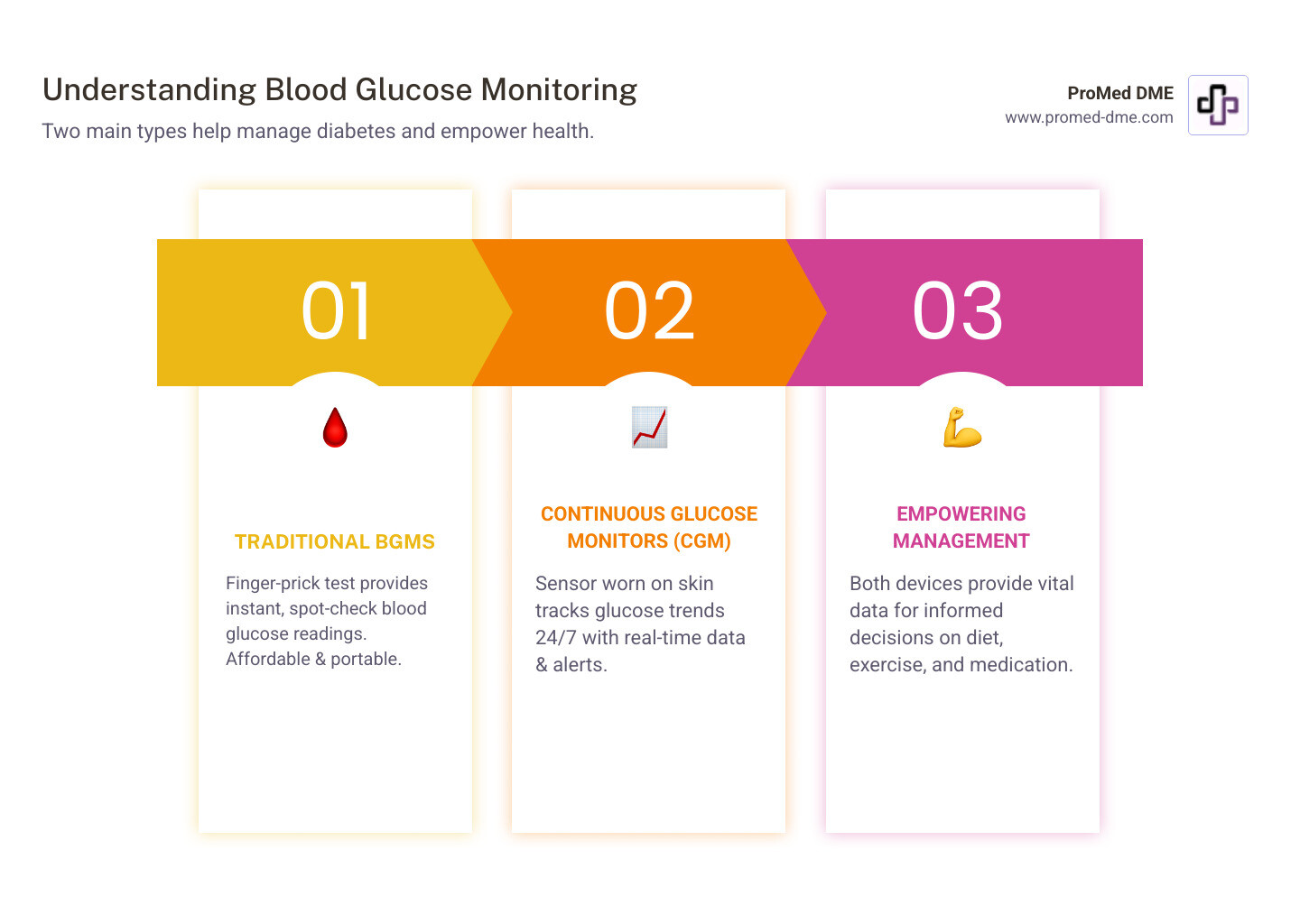
Types of Blood Glucose Monitors: Finding Your Fit
Choosing the right blood glucose monitoring device is a personal decision. Today's technology offers more choices than ever, from reliable traditional meters to smart continuous monitors. Let's explore your options to find the device that best fits your lifestyle.
Traditional Blood Glucose Meters (BGM)
Traditional meters have been a trusted tool in diabetes management for decades. This blood glucose monitoring device is likely what comes to mind when you picture checking blood sugar.

How it works: You insert a test strip into the meter, use a lancing device to get a tiny drop of blood from your fingertip, and touch the strip to the blood. Within seconds, your glucose level is displayed. It's a precise snapshot of your blood sugar at that moment.
Advantages: Traditional meters are portable, affordable, and provide immediate results for on-the-spot decisions about food or medication. When used correctly, they offer excellent accuracy trusted by doctors.
Trade-offs: Each reading provides only a single point in time, not the full picture of your glucose patterns. The required finger pricks can be uncomfortable, and the ongoing cost of test strips can add up.
Continuous Glucose Monitors (CGM)
CGMs transform diabetes monitoring from periodic checks to continuous awareness, acting like a health assistant that tracks your glucose levels day and night.
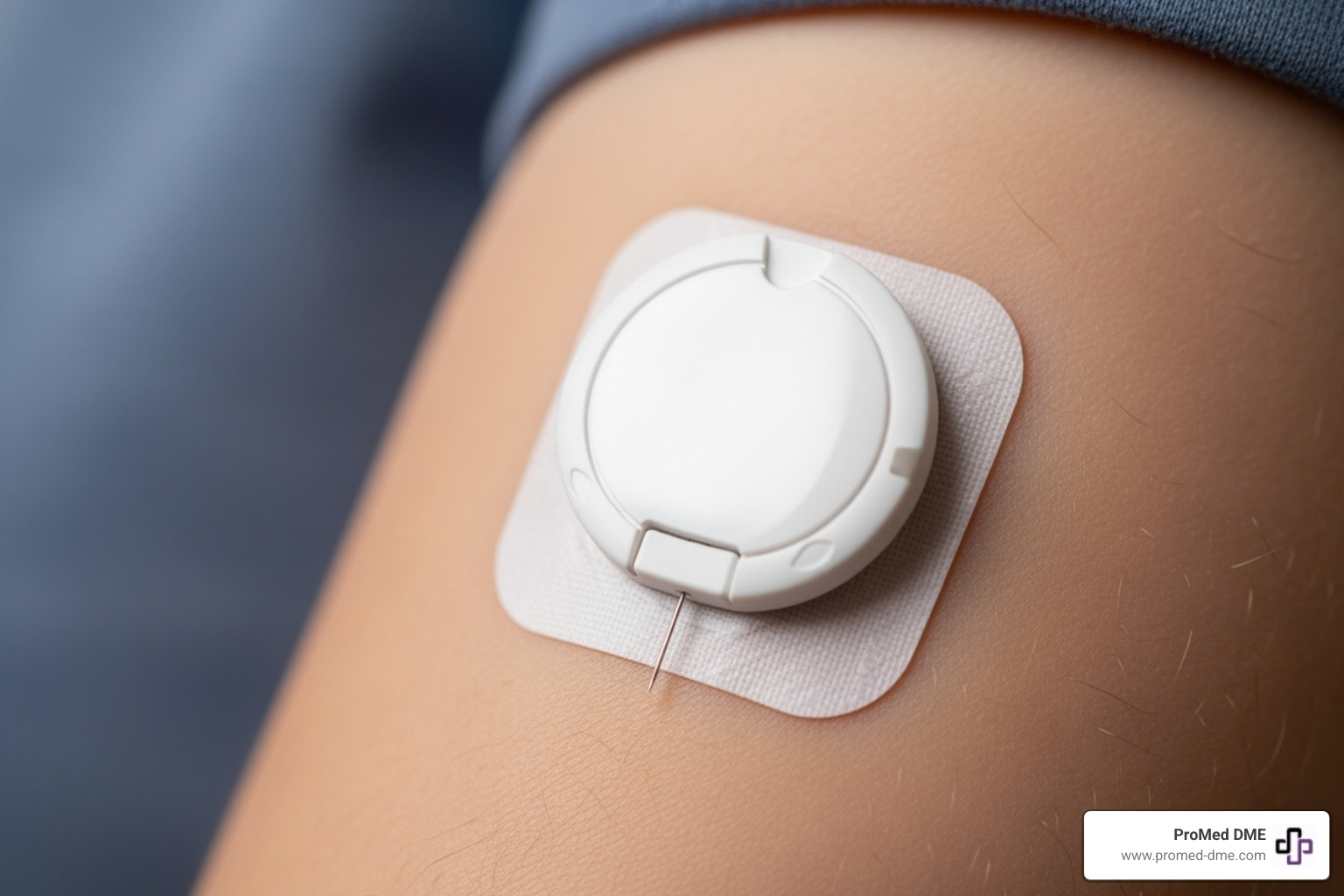
How it works: A small sensor sits just under your skin (usually on your arm or belly), measuring glucose in the fluid between your cells. It sends this information wirelessly to your phone or a separate device every few minutes, showing your glucose story as it unfolds.
Advantages: The real-time data and trends are game-changing, showing how meals and activities affect you. Alerts for high and low levels act as a safety net, which is especially valuable for those with hypoglycemia unawareness. Best of all, CGMs dramatically reduce the need for daily finger pricks.
Considerations: CGMs have a higher upfront cost, though insurance coverage is improving. You must wear the sensor continuously and replace it every 7-14 days. There's also a slight time lag in readings compared to a finger-stick test. For more details on this technology, Dexcom's guide is a great resource.
BGM vs. CGM: A Side-by-Side Comparison
Seeing the differences side-by-side can help clarify which blood glucose monitoring device might be best for you:
| Feature | Traditional Blood Glucose Meter (BGM) | Continuous Glucose Monitor (CGM) |
|---|---|---|
| How it works | Measures glucose in blood from finger prick | Measures glucose in tissue fluid via worn sensor |
| Data provided | Single reading at testing time | Continuous readings every few minutes with trends |
| Frequency | When you choose to test | Automatic monitoring 24/7 |
| Pain level | Finger prick each time | Initial sensor insertion, then painless |
| Cost | Lower device cost, ongoing strip expenses | Higher upfront cost, periodic sensor replacement |
| Conveniencia | Quick spot checks anywhere | Constant monitoring with smartphone alerts |
| Best for | Confirming readings, making immediate decisions | Understanding patterns, catching highs/lows early |
The choice isn't about the "best" device, but the right one for your diabetes journey.
How to Choose the Right Blood Glucose Monitor
Picking the right blood glucose monitoring device requires matching it to your daily routine, budget, and comfort. There's no single "best" monitor; the right fit is a personal choice. Thinking through your specific needs makes all the difference.
Key Factors to Consider When Selecting a Device
Here is a checklist of what really matters when choosing your blood glucose monitoring device:
- Insurance coverage: Start by calling your insurance company. Find out which meters, test strips, and CGM systems they cover, as benefits vary significantly between plans.
- Cost of supplies: The ongoing cost of test strips or CGM sensors can be more significant than the device's price. Factor this into your long-term budget.
- Ease of use: A device you use daily should be comfortable and simple. Look for a clear, easy-to-read screen, a comfortable size, and a small blood sample requirement.
- Data storage and connectivity: Many modern meters store hundreds of readings and connect to smartphone apps. These features help you log numbers, see averages, and share data with your healthcare team. The Mayo Clinic's guide on choosing blood glucose meters offers more insight on these features.
- Special features: Don't overlook features like large buttons, audio prompts, or backlit screens, which can make daily monitoring much more manageable.
The Rise of Advanced Diabetes Technology
Diabetes technology is constantly advancing to make management easier.
- Smart insulin pens: These devices connect to smartphone apps to help track doses, calculate insulin needs, and send reminders. They offer connected benefits without the complexity of an insulin pump.
- Alternative site testing: Some meters allow testing on your palm or forearm, which can be more comfortable. However, fingertips provide the most accurate reading when your blood sugar is changing rapidly.
- Integrated systems: Also known as artificial pancreas systems, these combine CGMs with insulin pumps. The system uses CGM readings to automatically adjust background insulin, handling many of the constant micro-adjustments for you.
- Future innovations: Researchers are working on non-invasive monitoring and even more sophisticated automated systems, offering optimism for the future of diabetes care.
The best device is the one you will use consistently to manage your health. Sometimes the most advanced option isn't the best choice for your current lifestyle.
A Guide to Your Blood Glucose Monitoring Device and Its Use
Having the right blood glucose monitoring device is the first step; using it correctly is what open ups its benefits. With a little practice, you can get reliable readings to make confident health decisions every day.
How to Get an Accurate Reading Every Time
Consistent, accurate results come from following a few simple steps every time you test.
- Start with clean hands. This is a crucial step. Residue from food or lotion can throw off your reading. Wash with warm, soapy water and dry thoroughly.
- Use fresh test strips. Expired strips are unreliable. Always check the expiration date and use strips authorized for sale in your area, as the FDA warns against using unauthorized or pre-owned strips.
- Store supplies properly. Your blood glucose monitoring device and strips dislike extreme temperatures and moisture. Store them in a cool, dry place and keep the test strip vial tightly closed.
- Use control solution. This practice run for your meter ensures it's calibrated correctly. Use it when opening a new vial of strips, if you drop your meter, or if you get a questionable reading.
- Follow the instructions. Every meter is different. Your manual is the roadmap to accurate results, detailing the correct blood sample size and application method.
- Know when fingertips are best. While alternative sites can be more comfortable, fingertips provide the most up-to-the-minute reading. Stick with a fingertip test if you suspect a low or if your blood sugar is changing rapidly. The CDC offers more excellent tips for accuracy.
Maintaining Your Blood Glucose Monitoring Device
A little care goes a long way in keeping your meter reliable.
- Mind the temperature. Avoid leaving your meter in a hot car or freezing garage. Room temperature is ideal.
- Keep it clean. Wipe your meter with a soft, slightly damp cloth. Clean off any blood promptly.
- Protect test strips. Air and moisture can ruin strips. Always replace the cap on the vial immediately.
- Use authorized supplies only. Using strips not made for your meter or bought from questionable sources is dangerous. The FDA has issued a strong safety communication on this topic, as incorrect readings can lead to harmful treatment decisions.
Troubleshooting: What to Do with Unexpected Results
Even with perfect technique, you might get an odd result or error code. Don't panic.
- Error Codes: Check your user manual to understand what the code means. If the problem persists, call the manufacturer's customer support.
- Unexpected Readings: If a number doesn't seem right, wash your hands and test again. If it's still strange, use control solution to check your meter and strips.
- Consider Context: Think about recent meals, exercise, stress, or medication changes that could be affecting your blood sugar.
- When to Call for Backup: If a CGM reading doesn't match your symptoms, use your traditional meter for a fingerstick test to verify before making treatment decisions.
- When to Call Your Doctor: If you consistently get readings that don't make sense or are unsure how to respond, contact your healthcare provider.
Understanding Your Results and Taking Action
Getting a number from your blood glucose monitoring device is just the start. The real power is in understanding what that number means and how to act on it.
What Are Normal Blood Glucose Ranges?
While there are general guidelines, your individual goals matter most. Your healthcare provider will set personalized targets based on your unique situation.
- General Guidelines: For adults without diabetes, the American Diabetes Association suggests a fasting blood glucose below 100 mg/dL and below 140 mg/dL two hours after meals.
- Personalized Goals: If you have diabetes, your doctor will set specific target ranges based on your age, health, medications, and type of diabetes. It's vital to work with your doctor to establish and review these goals.
- A1C (Glycated Hemoglobin): Your daily monitoring provides the data that contributes to your A1C, which is an average of your blood glucose over the past 2-3 months. Consistent monitoring helps you and your doctor understand the daily fluctuations that create that average. You can find more detailed information in the American Diabetes Association guidelines.
How Often Should You Test?
The ideal testing frequency is as individual as you are and should be discussed with your healthcare provider. Several factors influence how often you should test:
- Type of Diabetes & Medications: People with Type 1 diabetes or those on insulin generally need to test more often to make dosing decisions and prevent low blood sugar.
- Meals & Exercise: Testing before and after meals or physical activity helps you understand how they impact your glucose levels, empowering you to make better choices.
- Illness or Stress: When you're sick or stressed, your levels can fluctuate unexpectedly, making more frequent monitoring important.
- Changes in Routine: If you change your diet, activity level, or medication, temporarily increase testing to see how your body responds.
- Symptoms: Always test immediately if you experience symptoms of high or low blood sugar to confirm what's happening and guide your next steps. CGMs are particularly valuable for providing alerts, especially if you don't always recognize symptoms.
The goal is to use this information to make informed decisions that help you stay within your target range and manage your diabetes effectively.
Frequently Asked Questions about Blood Glucose Monitoring
Managing diabetes brings up many questions. Here are straight answers to the most common ones we hear about using a blood glucose monitoring device.
Can I reuse my lancets or test strips?
Let's be crystal clear: absolutely not.
Reusing supplies is unsafe. A lancet dulls after one use, making the next prick more painful and increasing your risk of infection. A test strip contains chemicals for a one-time reaction; reusing it will give an inaccurate reading and could damage your meter. For safety, the FDA warns against using any pre-owned or unauthorized supplies. Your health is worth the cost of fresh, single-use lancets and strips.
How accurate are home blood glucose monitors?
Modern home blood glucose monitoring device units are very accurate when used correctly and meet strict regulatory standards. However, accuracy depends on you.
Common mistakes that cause inaccurate readings include not washing your hands before testing or using expired or improperly stored test strips. Certain medications, severe dehydration, and extreme temperatures can also affect results. To ensure your device is working correctly, use control solution regularly, especially if you get a reading that doesn't match how you feel.
What's the difference between a blood sample and a CGM reading?
Understanding this difference is key to good diabetes management.
A traditional finger-stick meter measures glucose directly from your capillary blood. This provides a real-time, "gold standard" reading that is best for immediate treatment decisions.
A CGM measures glucose in your interstitial fluid—the liquid surrounding your cells. Because glucose moves from the blood into this fluid, there is a slight time lag of a few minutes.
This lag matters most when your glucose is changing rapidly, such as after a meal or exercise. In these situations, your CGM reading might be a few minutes behind your actual blood sugar. This is why CGM manufacturers recommend confirming with a finger-stick test if your symptoms don't match your CGM reading. Both technologies are valuable: finger-sticks for precise, in-the-moment decisions, and CGMs for trends, patterns, and alerts.
Conclusion: Empowering Your Health Journey
Managing diabetes is an achievable goal. We've explored blood glucose monitoring device options, from traditional meters to innovative CGMs. Each can help you understand your body and make informed health decisions.
The most important takeaway is that consistency beats perfection. The best blood glucose monitoring device is the one you will use every day. It becomes your partner, providing the information you need to live confidently with diabetes.
Your monitor is your compass, guiding daily decisions about food, exercise, and medication. The data you collect helps you and your healthcare team fine-tune your management plan.
Taking control starts with the right tools and support. At ProMed DME, we simplify the process of getting your diabetes supplies. Based in Stuart, Florida, we ship across the United States and are committed to providing exceptional customer service. We have a dedicated nurse on staff to answer your questions, we work with most insurance plans to minimize your costs, and we offer free shipping.
Your health journey is unique, but you don't have to steer it alone. With the right monitoring device and a trusted partner for your supplies, you can take confident steps toward better diabetes management.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.




