Sugar Tracking Made Simple: Best Blood Glucose Monitoring Systems

What is a Blood Glucose Monitoring System and Why is it Essential?
A blood glucose monitoring system is a medical device that measures blood sugar (glucose). It's a vital tool for people with diabetes to track their levels at home, helping them manage their condition and prevent complications.
Key types of blood glucose monitoring systems:
- Traditional Blood Glucose Meters (BGMs): Require a finger prick and test strip for each reading.
- Continuous Glucose Monitors (CGMs): Use a small sensor under the skin for real-time readings.
- Intermittently-Scanned CGMs (isCGMs): Require scanning a sensor to get readings.
These systems are recommended for:
- People with Type 1 or Type 2 diabetes
- Those with gestational diabetes
- Anyone advised by a doctor to monitor blood sugar
Research like the Diabetes Control and Complications Trial has proven that regular home monitoring is essential for good glucose control and leads to fewer complications. These devices test either a drop of blood or the fluid under your skin, providing results that guide decisions about food, exercise, and medication. Choosing the right system depends on your lifestyle, budget, and monitoring needs.
The Main Types of Blood Glucose Monitoring Devices
Choosing a blood glucose monitoring system means picking the right tool for your lifestyle. The two main types, traditional blood glucose meters (BGMs) and continuous glucose monitors (CGMs), both track your blood sugar but offer unique advantages.

How Traditional Blood Glucose Meters (BGMs) Work
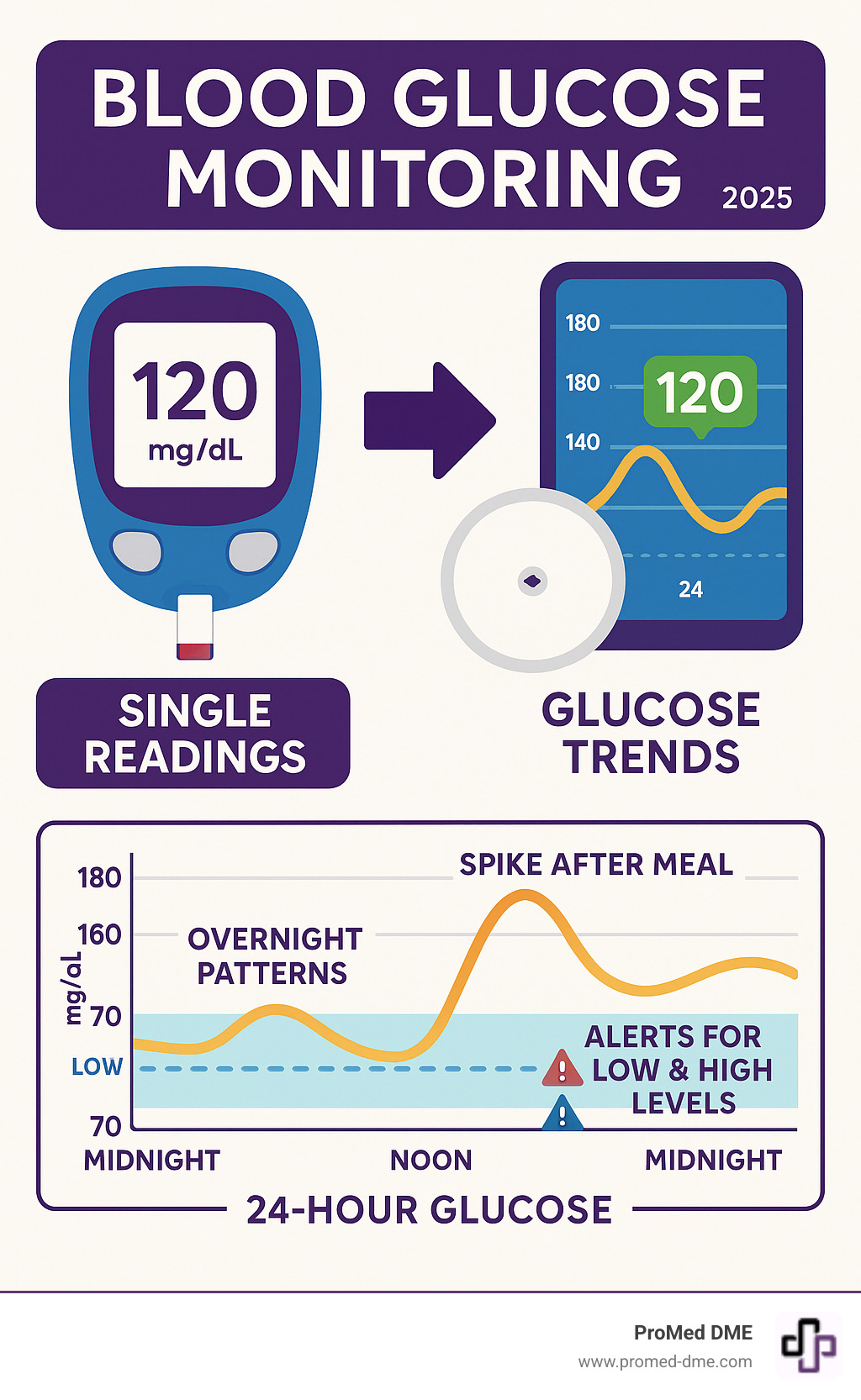
For decades, traditional blood glucose meters have been a reliable choice. These portable devices provide a precise snapshot of your glucose at a specific moment. The process uses the finger-prick method: a lancet creates a tiny puncture on your fingertip for a small blood sample. You apply this blood to a test strip inserted in the meter. Within seconds, the meter reading appears, usually in milligrams per deciliter (mg/dL). The main appeals of BGMs are their affordability and portability. However, they only provide point-in-time data, meaning you see a single moment's reading, not the overall trend.
How Continuous Glucose Monitors (CGMs) Work
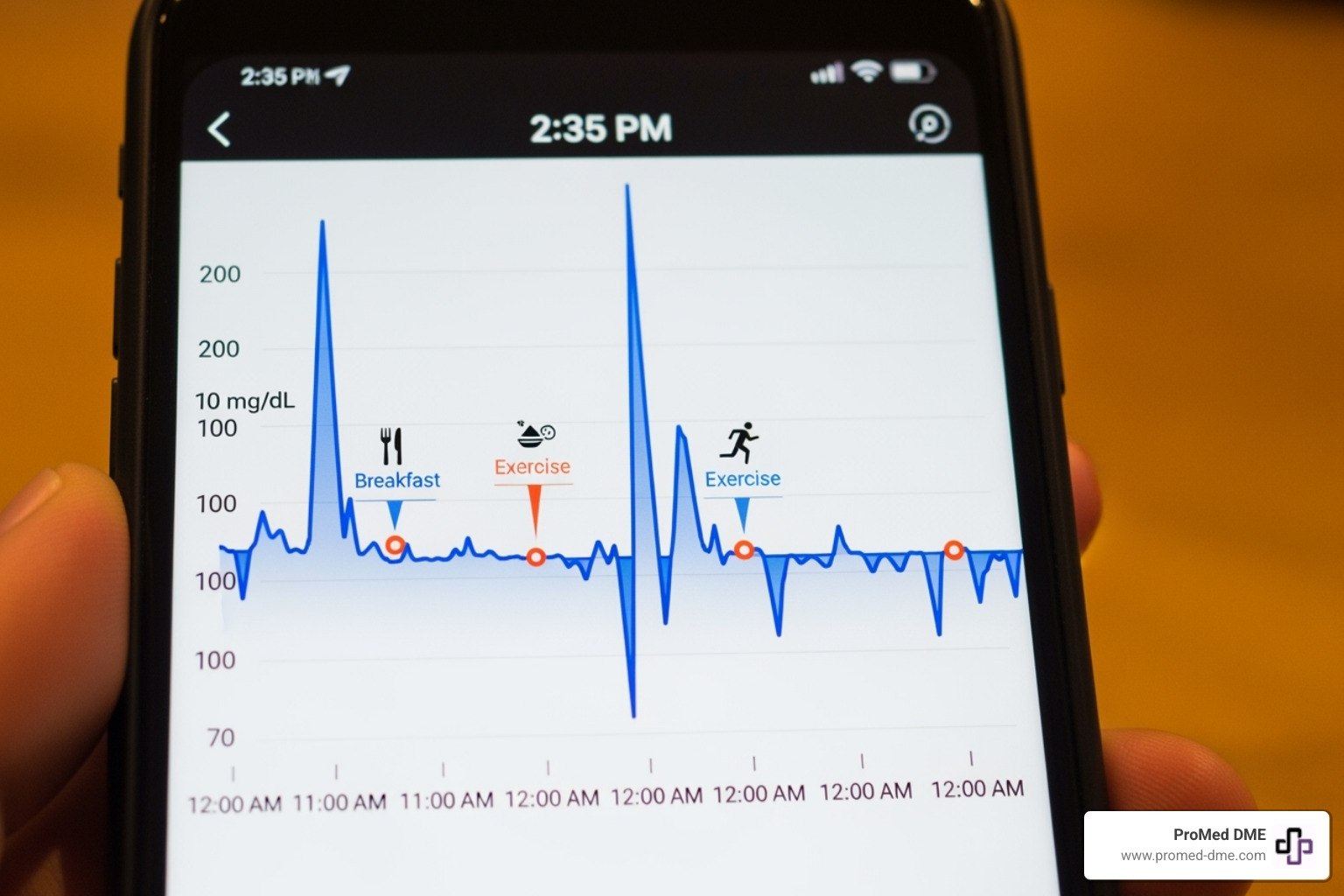
Continuous glucose monitors are a leap forward in diabetes tech, providing a continuous stream of glucose data. The system uses a small wearable sensor inserted just under the skin (on the arm or abdomen) to measure glucose in the interstitial fluid (the fluid around your cells). This reading closely tracks blood glucose, though there can be a 5-10 minute lag. A transmitter sends data wirelessly to a receiver or smartphone app, giving you real-time data and trend arrows that show if your glucose is rising or falling. Key features include customizable alarms for high and low levels and no finger pricks for readings for daily monitoring. Sensors last 7 to 15 days and require a brief warm-up period after application. CGMs offer game-changing insights into glucose patterns that traditional meters can't provide.
How to Choose the Right Blood Glucose Monitoring System for You
Choosing the right blood glucose monitoring system requires thinking about your budget, needs, and daily routine. Whether you prefer advanced technology with lots of data or a simple, straightforward device, there's a system that will work for you.

Key Factors to Consider When Selecting a Device
Consider these practical factors when choosing a device:
- Cost considerations: Look beyond the upfront price of the meter to the ongoing cost of supplies. For BGMs, this means test strips for each reading. For CGMs, it's sensor replacements every 7-15 days.
- Insurance coverage: Check what your plan covers. Medicare Part B, for example, covers monitors prescribed by a doctor. At ProMed DME, we specialize in working with Medicare, Medicaid, and commercial insurance to minimize your out-of-pocket costs.
- Ease of use: Think about screen readability, button size, and other features like audio readings that can make daily testing more comfortable.
- Technology and connectivity: Many devices connect to smartphone apps to track and share data. Decide if you prefer digital tracking or a simpler, non-connected device.
- Special features: Look for features that suit your needs, such as alternate site testing, fast reading times, large data storage, or the predictive alerts and trend arrows offered by CGMs.
Matching a System to Your Lifestyle and Needs
Your lifestyle should guide your choice.
- Traditional blood glucose meters (BGMs) are ideal for those who prefer straightforward, simple monitoring. They are perfect if you check your glucose a few times a day and value simplicity, or if you need a reliable backup for a CGM.
- Continuous glucose monitors (CGMs) are best for understanding the bigger picture. They provide valuable insights if you're active, want to see how food and exercise affect you, or need help avoiding highs and lows. The alarms are especially helpful if you have trouble sensing when your glucose is dropping.
Consider your comfort with technology. Some people love data streaming to a smartphone, while others prefer the simplicity of checking when they choose. For more information, the National Institutes of Health offers excellent resources.
The Importance of Your Healthcare Provider's Recommendation
Choosing a blood glucose monitoring system is a medical decision that should be made with your healthcare team. Your doctor or diabetes educator understands your specific needs and will help you:
- Establish personalized glucose targets: Your targets depend on your type of diabetes, medications, and health goals.
- Determine monitoring frequency: How often you check depends on your diagnosis and treatment plan (e.g., if you take insulin).
- Get a prescription: A prescription is essential for insurance coverage and ensures you get a medically appropriate device.
Your provider can also offer hands-on training to ensure you use your device correctly for the most accurate and reliable readings.
A Closer Look at Continuous Glucose Monitoring (CGM)
Continuous glucose monitoring (CGM) has revolutionized diabetes management. Instead of single-point finger pricks, these blood glucose monitoring systems provide a constant stream of data, turning guesswork into clear, actionable information. A CGM acts like a personal glucose detective, showing you the complete picture of how your body responds to food, activity, and medication.
The Major Advantages of Using a CGM
CGMs allow you to be proactive rather than reactive in your diabetes management. Key advantages include:
- Real-time feedback: See how food and exercise affect your glucose in the moment, allowing for better, faster decisions.
- Reduced finger-sticks: The daily routine of multiple finger pricks is eliminated, though occasional confirmation checks may be needed.
- High and low alerts: Customizable alarms can warn you of dangerous glucose levels, even while you sleep, which is vital if you have trouble sensing these changes.
- Understanding trends: Find patterns in your glucose levels to help you and your provider fine-tune your management plan.
- Improved A1c levels: Studies show that the detailed insights from CGMs often lead to better overall glucose control and lower A1c levels.
- Peace of mind: Knowing your glucose is being monitored 24/7 can significantly reduce diabetes-related anxiety.
Potential Drawbacks and Limitations of CGMs
While CGM technology is powerful, it's important to be aware of potential limitations:
- Cost: Sensors need regular replacement (every 7-15 days), which can be expensive. However, insurance coverage is improving, and ProMed DME can help steer plans to minimize your costs.
- Insurance problems: Coverage can be complex, sometimes requiring prior use of traditional meters or limiting brand choice.
- Sensor lifespan and warm-up time: Each sensor has a limited life and requires a warm-up period (30 minutes to 2 hours) before providing data.
- Skin irritation: Some users experience redness or itching at the sensor site. Rotating sites and using special adhesives can help.
- Data lag: There's a short delay (a few minutes) between blood glucose changes and the CGM reading, which is important during rapid fluctuations.
- Information overload: The constant data stream can feel overwhelming initially. It takes time to learn how to interpret the trends without stress.
- Calibration needs: While many CGMs don't require calibration, you should still confirm with a finger-stick test if readings don't match your symptoms.
Most users find the benefits outweigh these challenges, especially with support from a healthcare team and a knowledgeable supplier.
Ensuring Accuracy and Proper Use of Your Device
Accurate readings from your blood glucose monitoring system are essential for your health and safety. Inaccurate results can lead to dangerous treatment decisions, so it's crucial to ensure you're getting the most reliable data possible.

Best Practices for Your blood glucose monitoring system
Following these simple habits can dramatically improve accuracy:
- Wash your hands: Always wash and dry your hands thoroughly before testing. Food, lotion, or oils can affect your reading.
- Properly store supplies: Test strips are sensitive to moisture, light, and extreme temperatures. Keep the vial closed and store supplies as instructed.
- Never share equipment: To prevent the spread of blood-borne pathogens, your monitoring system is for your use only.
- Use authorized, unexpired supplies: Only use test strips and sensors made for your device that are not expired. The FDA warns that unauthorized strips can give dangerously inaccurate results.
- Use control solution: Test your meter with control solution when opening new strips, if you drop the meter, or if readings seem off.
The CDC offers more guidance on accurate monitoring at https://www.cdc.gov/diabetes/diabetes-testing/monitoring-blood-sugar.html.
Understanding and Verifying Your blood glucose monitoring system
Knowing when to trust or double-check your readings is a key skill.
- Testing location matters: Alternate sites (palm, forearm) are less painful than fingertips but also less accurate when glucose is changing rapidly. Always use fingertips after meals, during illness, after exercise, or if you feel symptoms of a high or low. Never use alternate site results for insulin dosing or CGM calibration.
- Verify CGM readings when needed: While CGMs are accurate, confirm with a finger-stick test if the reading doesn't match how you feel, if the device prompts you, or if you have symptoms of a high or low.
- Compare with your healthcare team: Bring your meter to appointments to compare its results with lab tests and get feedback on your technique.
When to Contact Your Healthcare Provider
Don't hesitate to contact your healthcare provider in these situations:
- Consistently high or low readings: If your levels are frequently outside your target range, your treatment plan may need adjustment.
- Readings don't match symptoms: If your device shows normal readings but you feel unwell (or vice versa), trust your body and call your provider.
- Device malfunctions: If your device displays errors or acts up, call the manufacturer's support line. If the issue persists, contact your provider.
- Questions about treatment: Always ask your provider if you're unsure how to interpret readings or adjust treatment.
Seek immediate medical attention for any blood glucose-related emergency.
Frequently Asked Questions about Blood Glucose Monitoring
Here are answers to some common questions about blood glucose monitoring systems.
What should my glucose levels be?
This is a common question, but the answer is personal. While general ranges exist for adults without diabetes (fasting below 100 mg/dL; after eating below 140 mg/dL), your targets will be different if you have diabetes. Your age, health, and treatment plan all factor in. Your healthcare provider is the only one who can set your personal glucose targets. While the American Diabetes Association offers general guidelines, always follow your doctor's specific recommendations.
Can I test from sites other than my fingers?
Yes, many traditional blood glucose monitoring systems allow Alternate Site Testing (AST) from your palm, forearm, thigh, or calf, which can be less painful than using fingertips. However, there's a catch: blood flow to these sites is slower, so readings can lag 10-20 minutes behind your actual blood glucose.
Always use your fingertip in these situations:
- When blood sugar may be changing rapidly (after meals, exercise, insulin, or during illness).
- If you suspect high or low blood sugar.
- If the reading doesn't match how you feel.
- For any insulin dosing decisions or CGM calibration.
Fingertip testing remains the gold standard for accuracy in critical moments.
Are used or unauthorized test strips safe to use?
No, they are not safe. The FDA has issued serious warnings against using previously owned, unauthorized, or expired test strips.
The risks are severe:
- Inaccurate readings: This can lead to dangerous treatment decisions, like taking the wrong dose of insulin.
- Contamination: Used strips could be contaminated with bloodborne diseases.
- Device damage: Improperly stored or incompatible strips can damage your meter.
- Unreliability: The chemicals on expired strips break down, making results untrustworthy.
While saving money is tempting, your health and safety are not worth the risk. Always use new, sealed, unexpired test strips that are compatible with your meter. Learn more from the FDA safety communication on test strips.
Conclusion: Taking Control of Your Health Journey
Managing diabetes can feel empowering with the right blood glucose monitoring system. This device is your personal health companion, providing the data you need to make smart, confident decisions about your food, exercise, and medication.
The journey to better health starts with informed choices. By understanding the different types of monitors and working with your healthcare team, you can select the system that best fits your life—whether it's a straightforward traditional meter or a CGM offering continuous insights. Consistent, accurate monitoring is what matters most.
While your healthcare provider is your primary ally, you shouldn't have to steer the complexities of supplies and insurance alone. That's where ProMed DME comes in. Based in Stuart, Florida, we ship top-quality diabetes supplies across the United States, simplifying the process for you. We work with most insurance plans, including Medicare and Medicaid, to minimize your costs and offer free shipping. We even have a dedicated nurse on staff to provide extra support.
Let us handle the supplies so you can focus on living your healthiest life.
Ready to simplify your diabetes management? Visit us at https://www.promed-dme.com to get started.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.



