What Medicare Covers for Wound Care Supplies (and What It Doesn't)

Navigating Medicare for Your Wound Care Needs
Proper wound care is crucial for healing, especially as we age or manage health conditions like diabetes. However, understanding what medicare wound care supplies are covered can be a puzzle. Many beneficiaries struggle to determine what their plan pays for, how to get the right supplies, and what the final cost will be.
This guide will simplify Medicare's rules for wound care, helping you get the supplies you need and avoid unexpected bills. Here's a quick overview:
- Medicare Part B covers medically necessary "surgical dressings" for wounds caused by surgery or that require debridement (unhealthy tissue removal).
- Covered supplies include primary dressings (gauze, hydrogel, foam) and secondary dressings (tape, bandages).
- Medicare Part A covers supplies during an inpatient stay at a hospital or skilled nursing facility (SNF).
- Medicare Advantage (Part C) plans must offer at least the same coverage as Original Medicare, but may have different rules and extra benefits.
- What's NOT covered: Everyday items like adhesive bandages (Band-Aids) or antiseptic creams you purchase yourself at a store are typically not covered.
We'll break down what's covered, what's not, and how different Medicare plans handle wound care.

Learn more about medicare wound care supplies:
Understanding Medicare's Wound Care Coverage Rules
Medicare covers wound care and supplies that are deemed "medically necessary." This term has a specific meaning within Medicare's guidelines and often depends on the type of wound you have and the care it requires.
What is a "Qualifying Wound" for Medicare?
For Medicare to cover your medicare wound care supplies, your wound must be a "qualifying wound." This generally means the wound fits one of these descriptions:
- Caused by a surgical procedure: An incision from an operation, like a hip replacement or heart surgery, typically qualifies.
- Treated by a surgical procedure: A wound that requires stitches or other surgical intervention to close it can become a qualifying wound.
- Has undergone debridement: If a wound requires debridement—the removal of unhealthy tissue—it can qualify for coverage of necessary medicare wound care supplies. This is a critical step for many wounds to heal properly.
Common types of wounds that often meet these criteria include:
- Venous ulcers
- Diabetic foot ulcers
- Pressure ulcers (bedsores)
Coverage is for wounds that require professional treatment and specialized dressings, not just a simple bandage. Your doctor's clear documentation of the wound's nature and the medical necessity for the supplies is essential.
For more detailed information, you can refer to the official Provider compliance tips for surgical dressings [Fact sheet].
The Role of Debridement in Coverage
Debridement is the medical process of removing unhealthy, dead, or infected tissue from a wound. This process is vital for promoting healing and preventing infection. If your wound requires debridement, it helps establish it as a "qualifying wound" for Medicare coverage of related medicare wound care supplies.
Healthcare providers perform debridement in several ways:
- Surgical debridement: A doctor uses tools like a scalpel to remove unhealthy tissue.
- Mechanical debridement: Involves physically removing tissue, sometimes with special dressings or irrigation.
- Autolytic debridement: Uses your body's own enzymes, aided by dressings that create a moist healing environment.
- Enzymatic debridement: A special cream or gel with enzymes is applied to dissolve dead tissue.
- Biosurgical debridement: Uses medical-grade maggots to eat away dead tissue while leaving healthy tissue untouched.
The debridement procedure itself is a covered medical service. The necessity of this procedure is what often opens the door for coverage of the ongoing medicare wound care supplies you'll need afterward.
Acute vs. Chronic Wound Coverage
Wounds are generally categorized as acute or chronic, but the core principle of "medical necessity" for Medicare coverage remains the same for both.
- Acute wounds occur suddenly (e.g., cuts, burns, surgical incisions) and are expected to heal in a predictable timeframe.
- Chronic wounds fail to heal as expected, often due to underlying health conditions like diabetes or poor circulation. They can persist for months or years.
Medicare's coverage for medicare wound care supplies applies to both acute and chronic wounds, as long as they meet the "qualifying wound" criteria. The main difference is often the duration and intensity of care. Chronic wounds typically require more prolonged and complex management, as highlighted in research on the Challenges in the Treatment of Chronic Wounds, making reliable access to supplies even more critical.
What Wound Care Supplies and Services Does Medicare Cover?
Once your wound qualifies for coverage, what specific medicare wound care supplies and services will Medicare pay for? Coverage depends on whether you receive care in an inpatient setting (like a hospital) or an outpatient setting (at a doctor's office or at home).
Medicare Part B Coverage for Outpatient and Home Use
Medicare Part B (Medical Insurance) covers outpatient wound care services and supplies. When a healthcare professional dresses your wound, Part B covers their services and the necessary medicare wound care supplies, often referred to as "surgical dressings."
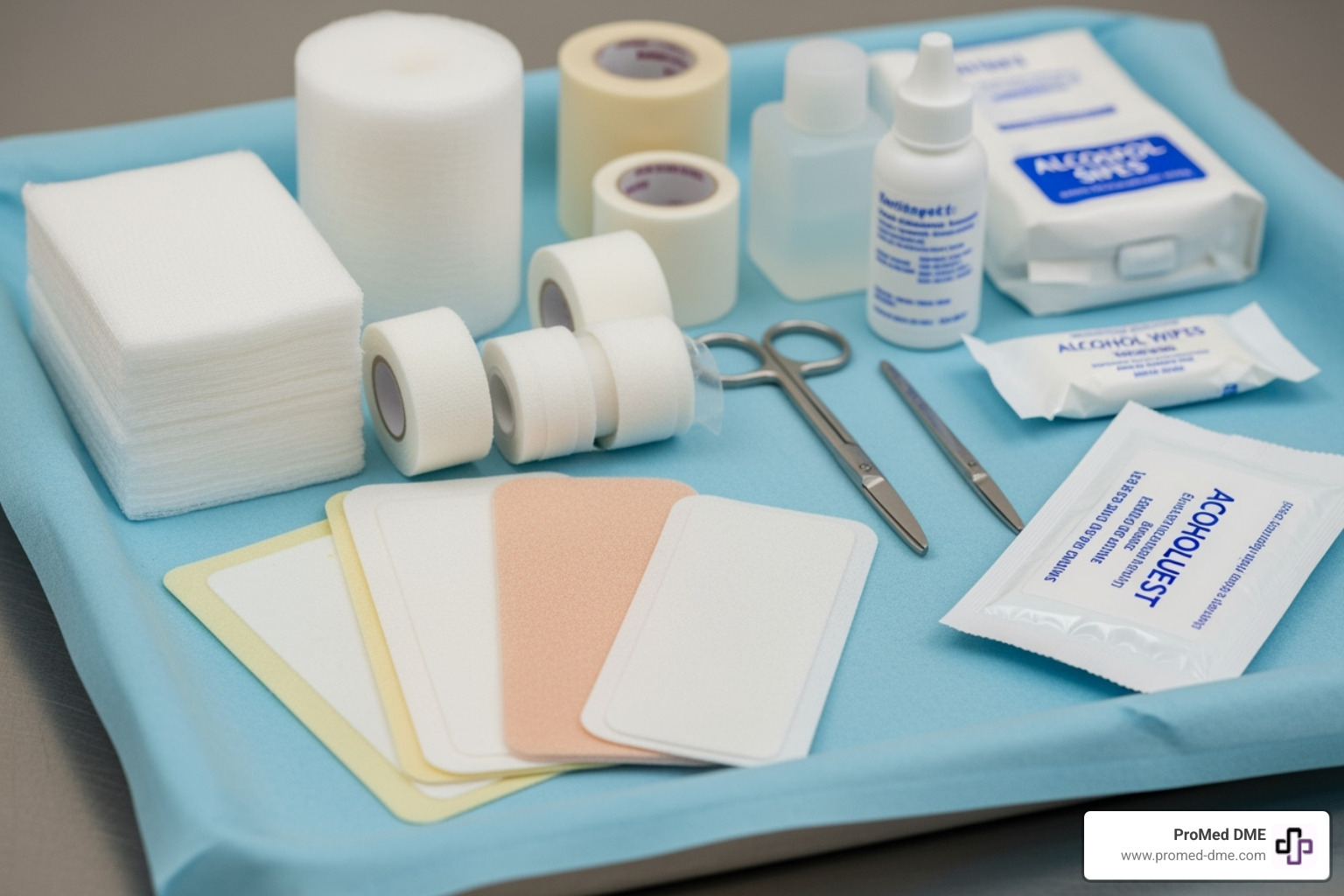
These dressings fall into two categories:
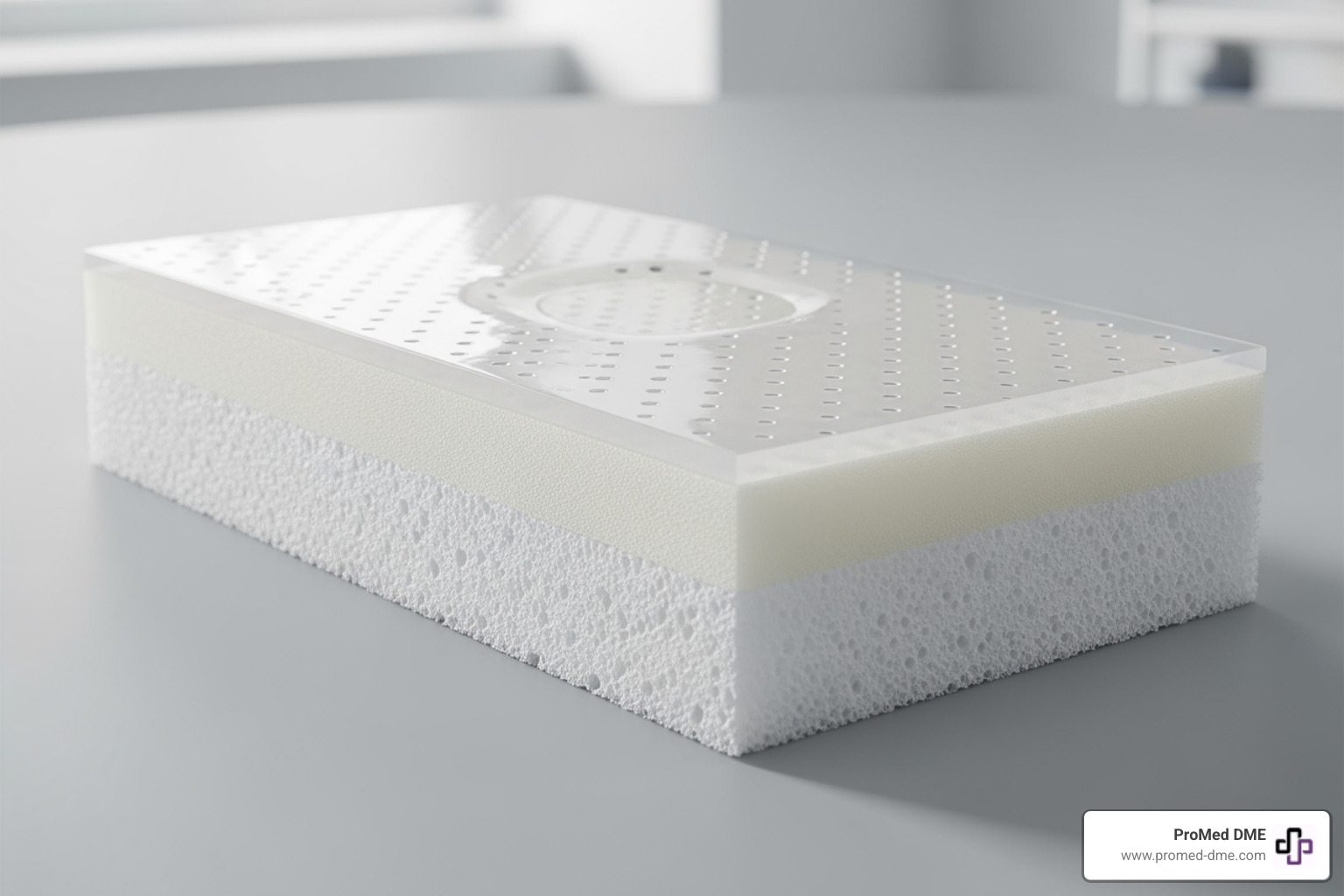
- Primary dressings: These are applied directly to the wound to aid healing. Examples include sterile gauze pads, hydrogel dressings, hydrocolloid dressings, alginate dressings, and foam dressings.
- Secondary dressings: These materials hold the primary dressing in place and add protection. Examples include adhesive tape, roll gauze, and bandages.
For these supplies to be covered, they must be medically necessary and part of a doctor's prescribed treatment plan for a qualifying wound. Simple first-aid items purchased over the counter are not covered.
For official details, Medicare.gov provides information on Surgical dressing services.
Advanced Therapies and Equipment
For complex wounds, advanced therapies can significantly speed up healing. Many are covered by Medicare Part B as Durable Medical Equipment (DME) when medically necessary.
- Negative Pressure Wound Therapy (NPWT): Also known as Vacuum-Assisted Closure (VAC) therapy, this uses a device to create suction over the wound, removing fluid and promoting tissue growth. Medicare Part B covers wound VAC when your doctor deems it necessary.
- Hyperbaric Oxygen (HBO) Therapy: This involves breathing pure oxygen in a pressurized chamber to increase oxygen in the blood, which boosts healing for certain wounds like diabetic foot ulcers.
- Electrical stimulation: This therapy applies low-level electrical currents to the wound to encourage cell growth and improve blood flow.
For more details on NPWT coverage, see the official guidelines: Medicare coverage for NPWT.
Medicare Part A Coverage in Hospitals and Skilled Nursing Facilities
When you are an inpatient in a hospital or a skilled nursing facility (SNF), Medicare Part A covers your wound care.
- Inpatient hospital stays: If you're admitted to a hospital, all necessary medicare wound care supplies and services are typically bundled into the hospital's payment from Medicare Part A. You won't be billed for individual dressings.
- Skilled Nursing Facility (SNF) care: Similarly, if you have a qualifying short-term stay in a SNF for rehabilitation or skilled nursing, Part A covers these services. Supplies are included in the daily rate Medicare pays the SNF. Coverage is limited: for a qualifying stay, days 1-20 have no out-of-pocket cost, but a daily coinsurance applies for days 21-100.
Navigating Your Costs for Medicare Wound Care Supplies
Understanding coverage is the first step; knowing your out-of-pocket costs is the next. Medicare has specific deductibles, premiums, and coinsurance that affect your total bill for medicare wound care supplies and services.

Costs with Original Medicare (Part A & B)
With Original Medicare, your costs depend on where you receive care.
Medicare Part A helps with inpatient services. For each benefit period in 2024, you must pay a $1,632 deductible. This covers your first 60 days in a hospital. For a qualifying skilled nursing facility (SNF) stay, days 1-20 are covered at $0, but from days 21-100, a daily coinsurance of up to $185.50 applies.
Medicare Part B covers outpatient services and medicare wound care supplies. In 2024, you must meet a $240 annual deductible and pay a monthly premium (typically $174.70). After your deductible is met, Medicare covers 80% of the approved amount, and you are responsible for the remaining 20% coinsurance.
| Cost Type | Medicare Part A (Inpatient) | Medicare Part B (Outpatient/Supplies) |
|---|---|---|
| Deductible | $1,632 per benefit period (2024) | $240 annually (2024) |
| Premium | Generally none (if you paid Medicare taxes for 10+ years) | $174.70 monthly (2024) |
| Coinsurance | Hospital: $0 for days 1-60, $408/day for days 61-90, etc. SNF: $0 for days 1-20, up to $185.50/day for days 21-100 (after 100 days, you pay all costs) | 20% of the Medicare-Approved Amount after deductible is met |
How Medicare Advantage (Part C) and Medigap Affect Costs
Other Medicare plans can change your out-of-pocket expenses for medicare wound care supplies.
Medicare Advantage (Part C) Plans are private plans that provide your Part A and B benefits. They must cover everything Original Medicare does, but they have different cost structures (deductibles, copayments) and often use provider networks. Many also offer extra benefits not covered by Original Medicare, like vision, dental, or over-the-counter allowances.
Medigap (Medicare Supplement Insurance) Plans work with Original Medicare to cover out-of-pocket costs like deductibles and the 20% coinsurance. A Medigap policy can significantly reduce your expenses for covered wound care services and supplies. You can learn more about How to compare Medigap policies to see how they might lower your costs.
What Wound Care is NOT Covered by Medicare?
It's important to know what Medicare typically does not cover to avoid unexpected bills.
Medicare generally does not cover:
- Custodial care: Non-medical, personal care that helps with daily activities like bathing, dressing, or eating.
- Common over-the-counter supplies: Basic items you buy at a drugstore, like adhesive bandages (Band-Aids), plain gauze for minor cuts, or antibacterial creams, are not covered if you purchase them yourself. Medicare's coverage is for prescribed "surgical dressings" from a Medicare-enrolled supplier.
- SNF stays beyond 100 days: Part A coverage for a SNF stay ends after 100 days per benefit period.
- Items that don't meet the "surgical dressing" definition: This can include products like skin sealants, wound cleansers, or certain antiseptics not integrated into a covered dressing.
The Essential Paperwork: How to Get Your Supplies Covered
Getting your medicare wound care supplies covered requires having the right documentation to prove medical necessity. This paperwork ensures you receive the appropriate supplies for your specific needs.

Specific Requirements for a Doctor's Order
For Medicare to cover your supplies, your doctor's order must be a written, signed, and dated document that is highly detailed. It must include:
- The type of wound (e.g., surgical, diabetic ulcer).
- The wound's exact location and size (length x width x depth).
- The specific type and size of dressing needed.
- The quantity of supplies required.
- The frequency of dressing changes (e.g., daily).
- The expected duration of need (e.g., "for 4 weeks").
This level of detail ensures the supplies you receive are perfectly matched to your treatment plan.
Ongoing Documentation and Coverage Limits for medicare wound care supplies
Coverage is not a one-time approval. It continues as long as there is a documented, ongoing medical need.
Your healthcare provider must conduct regular wound evaluations—typically monthly—to document the wound's progress (or lack thereof) and justify the continued need for medicare wound care supplies. These evaluations must record the wound's type, location, size, and amount of drainage. For patients in a SNF or with heavily draining wounds, weekly evaluations are often expected.
Your medical record must show the wound is improving or that the treatment plan is being modified if it is not. For most dressings, the order must be renewed at least every three months. This ensures your treatment plan is regularly reviewed. As long as medical necessity is clearly documented through these ongoing evaluations, Medicare will continue to cover reasonable and necessary supplies.
How to get medicare wound care supplies
Once you have a detailed doctor's order, you can get your supplies. Most medicare wound care supplies covered by Part B are provided through Durable Medical Equipment (DME) suppliers. It is critical that both your doctor and the DME supplier are enrolled in Medicare, or your claim may be denied.
In some cases, if you receive home health services, the home health agency may provide your wound care supplies as part of your care plan.
At ProMed DME, we simplify this process. We provide a wide range of high-quality medicare wound care supplies and work with most insurance plans, including Medicare, to minimize your costs. Our team helps verify your coverage and ensures you receive the supplies you need, delivered right to your door.
Frequently Asked Questions about Medicare Wound Care
Navigating wound care benefits can be confusing. Here are clear answers to some of the most common questions about medicare wound care supplies.
How does Medicare cover wound care in a skilled nursing facility?
In a skilled nursing facility (SNF), Medicare Part A is typically the primary payer, provided you have a qualifying 3-day prior inpatient hospital stay. Here's how coverage works for each benefit period:
- Days 1-20: Fully covered by Medicare Part A. You pay $0 out-of-pocket.
- Days 21-100: You are responsible for a daily coinsurance (up to $185.50 per day in 2024).
- After 100 days: Medicare Part A coverage ends, and you are responsible for all costs.
During a covered stay, all necessary medicare wound care supplies and services are bundled into the facility's payment from Medicare, so you won't receive separate bills for them.
Does Medicare cover vacuum-assisted closure (VAC) therapy?
Yes. Medicare Part B covers Negative Pressure Wound Therapy (NPWT), commonly known as wound VAC therapy, when your doctor determines it is medically necessary to treat your wound. Wound VAC systems are classified as Durable Medical Equipment (DME). After you meet your Part B deductible, Medicare generally covers 80% of the approved amount, and you are responsible for the remaining 20% coinsurance.
What common wound care items are not covered for home purchase?
Original Medicare does not cover common first-aid supplies that you buy over-the-counter for personal use. Medicare's coverage is for specialized, medically necessary items prescribed by a doctor, not everyday supplies.
Items typically not covered when you purchase them yourself include:
- Basic adhesive bandages (e.g., Band-Aids)
- Plain gauze and medical tape for minor cuts
- Topical antiseptic liquids (e.g., hydrogen peroxide) and over-the-counter antibiotic creams
Coverage for medicare wound care supplies applies specifically to "surgical dressings" prescribed for a qualifying wound and obtained from a Medicare-enrolled supplier.
Conclusión
We hope this guide has clarified the complexities of Medicare coverage for medicare wound care supplies. By understanding the rules, you can better steer your care and focus on healing.
The key takeaways are:
- Medicare covers supplies for a "qualifying wound"—one from surgery or that has been debrided.
- Proper documentation is essential. A detailed doctor's order and ongoing evaluations are the backbone of coverage.
- Know your plan. Whether you have Original Medicare, Medicare Advantage, or Medigap, understanding your specific costs is key to avoiding surprises.
At ProMed DME, we understand that dealing with a wound is stressful enough. Our mission is to make getting your supplies simple and worry-free. We offer top-quality medicare wound care supplies with exceptional customer service, including free shipping to your door, a dedicated nurse on staff for personalized support, and assistance with most insurance plans to minimize your costs. We aim to make your healing journey as smooth as possible.
Ready to simplify your wound care journey and get the supplies you need? Find how ProMed DME can be your trusted partner.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.