Pump or Pass? Identifying Ideal Candidates for Insulin Pump Therapy

Who Should Consider Insulin Pump Therapy?
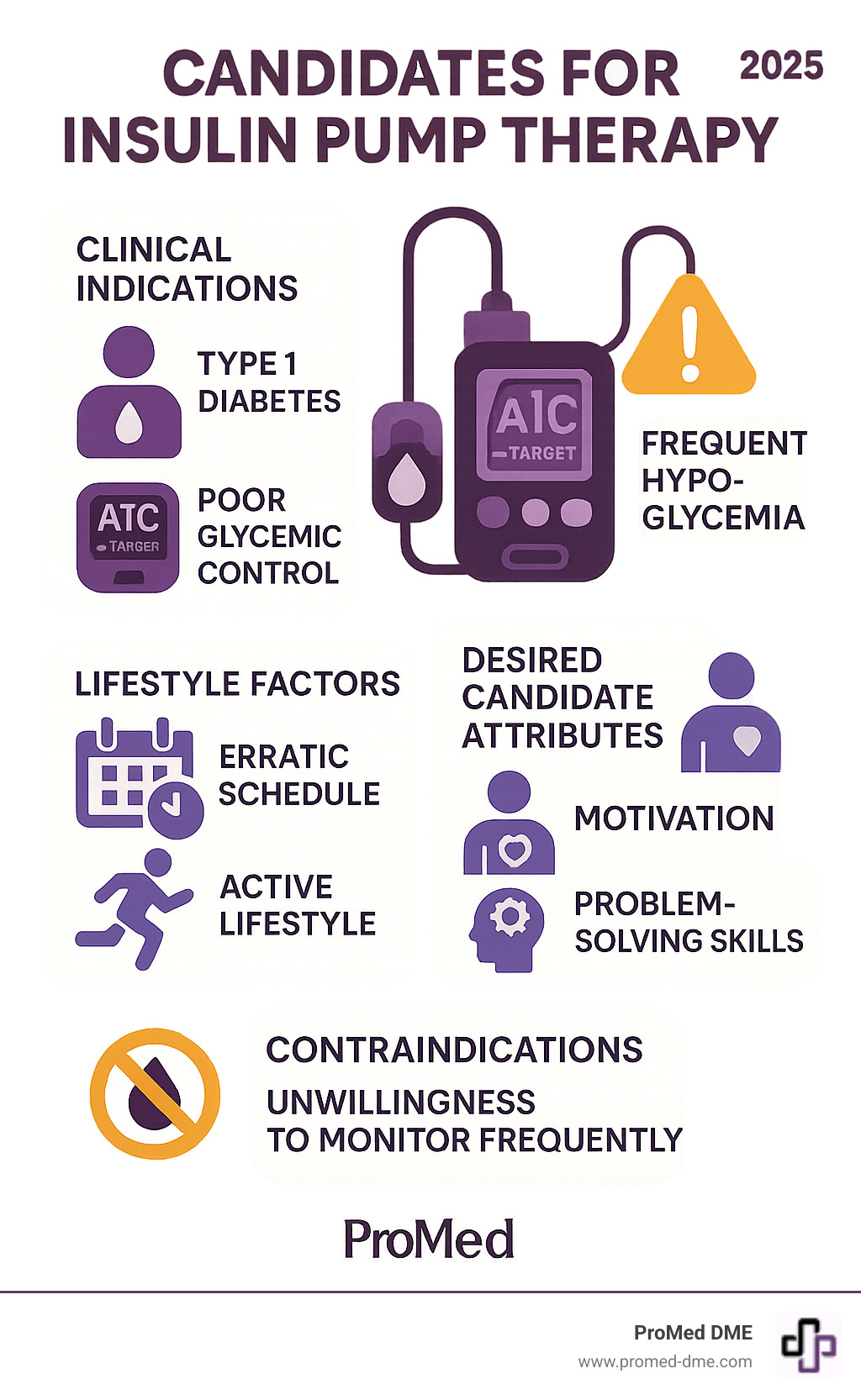
Candidates for insulin pump therapy are individuals who meet specific clinical, lifestyle, and personal criteria. Choosing a pump is a personal decision that requires careful assessment with your healthcare team.
Ideal candidates typically include:
- People with Type 1 diabetes or insulin-requiring Type 2 diabetes
- Those with poor blood sugar control despite multiple daily injections
- Individuals experiencing frequent or unpredictable low blood sugar episodes
- People with erratic schedules or active lifestyles requiring flexibility
- Those who are motivated and committed to frequent monitoring and learning
- Individuals with realistic expectations about pump therapy benefits and challenges
The decision to start pump therapy involves more than just having diabetes. Successful pump users are typically motivated, check their blood glucose levels several times a day, and have good problem-solving skills.
What makes someone a good fit? It's about matching the right person with the right technology at the right time. Active individuals who benefit from adjusting insulin during exercise, people with gastroparesis, women planning pregnancy, and those seeking more precise insulin dosing often find pumps life-changing.
However, pump therapy isn't for everyone. It requires commitment to safety protocols, frequent monitoring, and the willingness to learn new technology. The good news is that choosing pump therapy isn't a permanent decision—many people successfully switch between pumps and injections based on their changing needs.
Candidates for insulin pump therapy terms simplified:
- advantages and disadvantages of insulin pump therapy
- continuous glucose monitoring system
- how to use insulin pump therapy
Understanding Insulin Pump Therapy: The Basics
Insulin pump therapy, or continuous subcutaneous insulin infusion (CSII), is a modern way to deliver insulin that closely mimics your body's natural release. An insulin pump acts like a tiny, personal pancreas, delivering the precise amount of rapid-acting insulin your body needs, around the clock.
How Insulin Pumps Work
An insulin pump is a small, smart device that provides a continuous flow of insulin in two main ways, just like a pancreas:
- Basal Rate: This is your "background" insulin, a small, steady stream delivered continuously throughout the day and night. It covers your body's basic insulin needs, much like long-acting insulin from injections. Pumps can deliver these tiny amounts with incredible precision, sometimes as little as 0.025 units.
- Bolus Dose: This is your "on-demand" insulin, delivered manually to cover carbohydrates in meals or to correct high blood glucose. You tell the pump your carb count or current blood sugar, and its built-in calculator helps determine the exact dose.
Insulin travels from a reservoir inside the pump through a thin tube called an infusion set. At the end is a tiny, soft cannula, inserted just under your skin (often in the abdomen, thigh, or arm), where the insulin is absorbed. Most reservoirs hold enough insulin for two to three days.
CGM Integration and Closed-Loop Systems
The world of insulin pumps is always getting smarter. Today, most pumps available in the United States connect directly with Continuous Glucose Monitoring (CGM) technology. This connection provides your pump with real-time glucose readings, revolutionizing how insulin is delivered.
This powerful combination has led to advancements like automated insulin delivery and closed-loop systems (sometimes called "artificial pancreas" systems). These smart systems use advanced algorithms to automatically adjust insulin delivery based on your CGM data. They can predict where your glucose levels are headed and make tiny adjustments to your basal rates or give automatic correction boluses to help keep you in your target range. This can significantly reduce the constant worry and manual adjustments. You can dive deeper into this groundbreaking technology by exploring scientific research on automated insulin delivery.

As you can see, there are also different physical Types of Insulin Pumps available, from traditional tubed pumps to discreet tubeless patch pumps. These options offer choices to suit various lifestyles and preferences, ensuring candidates for insulin pump therapy can find a solution that fits their unique needs. We'll explore these options in more detail later!
Who Are the Ideal Candidates for Insulin Pump Therapy?
Deciding if insulin pump therapy is right for you is a personal decision made on your diabetes journey. It's not a one-size-fits-all solution. At ProMed DME, we believe the right approach requires a comprehensive assessment and close collaboration with your healthcare team.
Candidates for insulin pump therapy are individuals whose specific medical needs, lifestyle demands, and personal commitment align with what pump therapy offers. The key is matching the right person with the right technology at the right time.
Clinical Indications for Pump Use
Your healthcare provider might recommend pump therapy for several clinical reasons, as it can offer significant advantages over multiple daily injections.
Type 1 diabetes is the primary group for whom insulin pumps were designed. Since the body produces no insulin, the pump's ability to deliver precise, continuous doses can be life-changing, especially for children and teens.
People with Type 2 diabetes requiring multiple daily injections often find pumps helpful. If you're taking several insulin shots daily but still struggling to hit your blood sugar targets, a pump might be the missing piece.
Poor glycemic control despite your best efforts with injections is a strong indicator. Research shows pump users often achieve better A1C levels than those using multiple daily injections, with some studies showing improvements of nearly 1% in A1C values within 16 weeks.
If you experience frequent hypoglycemia or unpredictable low blood sugar, especially at night, a pump with modern safety features can be a game-changer. Features like "threshold suspend" can automatically stop insulin delivery when your glucose drops too low, reducing dangerous lows by 40-50%.
Hypoglycemia unawareness—where you don't feel the warning signs of low blood sugar—makes pump therapy with continuous glucose monitoring particularly valuable. The alerts can be lifesaving.
The dawn phenomenon, a natural blood sugar rise in the early morning, responds well to pump therapy. You can program higher basal rates during those specific hours.
Gastroparesis presents challenges with mealtime insulin timing. Pumps allow for extended or dual-wave boluses that deliver insulin gradually, better matching delayed food absorption.
During pregnancy or when planning to conceive, the tight blood sugar control needed for a healthy pregnancy often requires the precision that pump therapy provides.
For more detailed information, check out Who is a Candidate for Insulin Pump Therapy?.
Lifestyle Factors Favoring Pump Therapy
Beyond medical necessity, many candidates for insulin pump therapy find that pumps improve their quality of life through increased flexibility and convenience.
Active individuals and athletes love the ability to adjust or suspend insulin delivery during exercise. This flexibility can transform how you approach physical activity.
If you have erratic schedules or shift work, a pump adapts to your schedule rather than forcing your life to revolve around rigid injection times.
Frequent travelers appreciate how pumps handle time zone changes, varying activity levels, and unfamiliar foods with real-time adjustments.
Some people simply prefer the convenience over multiple daily injections, switching from 4-5 daily shots to one infusion site change every 2-3 days.
Needle phobia is a valid concern, and while pumps aren't needle-free, they dramatically reduce the frequency of needle sticks.
Desired Attributes of Successful Candidates for Insulin Pump Therapy
Having the right medical indication or lifestyle need is just the starting point. The most successful pump users share certain personal characteristics.
Motivation and commitment top the list. A pump is an amazing tool, but it's not a cure. The best users are genuinely excited to learn, troubleshoot, and actively participate in their diabetes management.
Realistic expectations matter. Pumps won't eliminate blood sugar checks or carbohydrate counting. Understanding what a pump can and cannot do prevents disappointment.
Problem-solving skills are handy for troubleshooting technical issues like failed infusion sites, bent cannulas, or alarms.
Technical comfort helps, though you don't need to be a tech wizard. If you're comfortable with smartphones, you'll likely adapt quickly.
Commitment to frequent monitoring is essential. Most healthcare providers and insurance companies require at least four blood glucose checks daily before starting pump therapy.
Carbohydrate counting proficiency is important for precise bolus dosing, but it's a skill that improves with practice.
Emotional stability and a strong support system from family, friends, and your healthcare team make the journey easier.
The physical ability to manage the device—including good vision and manual dexterity—is also important. For children, having capable and committed caregivers is essential.
Choosing pump therapy isn't permanent. Many people switch between pumps and injections based on their changing needs. The goal is finding what works best for you right now.
Weighing the Pros and Cons: Is a Pump Right for You?
Choosing an insulin pump is a personal decision. It's about balancing the potential benefits against the challenges to make an informed choice that aligns with your lifestyle and health goals.
Potential Benefits of Insulin Pump Therapy
For many, the advantages of pump therapy are compelling, leading to a significant improvement in both glycemic control and quality of life.
- Improved A1C and Better Glycemic Control: Studies show that pump therapy can lead to better blood sugar management than multiple daily injections (MDI). The precision of continuous basal insulin and fine-tuned boluses often results in lower A1C levels.
- Reduced Hypoglycemia Risk: Features like low glucose suspend (LGS) and predictive low glucose suspend (PLGS) can dramatically reduce the occurrence of severe or nocturnal hypoglycemia, providing immense peace of mind.
- Increased Lifestyle Freedom and Flexibility: This is a huge benefit. Pumps allow for spontaneous meals and exercise without rigid injection schedules. This flexibility is a major reason why many people who switch from MDI to a pump report an improved quality of life.
- Fewer Injections: Changing an infusion set every 2-3 days is a vast improvement over 4-5 daily injections, which is especially beneficial for those with needle phobia.
- Precise Dosing: Pumps deliver insulin in tiny increments, allowing for fine-tuning not possible with syringes or pens. This is particularly useful for children or individuals who are very sensitive to insulin.
- Access to Downloadable Data: Most pumps store detailed data on insulin delivery and glucose trends. This information can be uploaded and reviewed with your healthcare team to optimize your management plan.
You can dive deeper into these advantages by exploring resources like Benefits of Insulin Pump Therapy.
Potential Disadvantages and Challenges
It's equally important to understand the potential downsides of pump therapy. Being prepared for these can help prevent frustration.
- Risk of Diabetic Ketoacidosis (DKA): Because pumps only use rapid-acting insulin, any interruption in delivery (e.g., pump malfunction, infusion site issue) can quickly lead to DKA, a serious complication. A backup plan with injectable insulin is crucial.
- Infusion Site Failure: Issues at the infusion site are the most common problem. This can include bent cannulas, blockages, disconnections, or local infections.
- Constant Attachment to a Device: You'll be wearing the pump almost constantly. This can take getting used to and might affect clothing choices, intimacy, or certain activities.
- Skin Irritation and Adhesive Issues: The adhesive used for infusion sets can sometimes cause irritation or allergic reactions. Finding the right site and rotation strategy is important.
- Cost and Insurance Problems: Insulin pumps and their supplies can be expensive. While many insurance companies cover pumps, they often have specific criteria and may only pay for a new pump every four years. Ongoing supply costs can also add up.
- Technical Learning Curve: While modern pumps are user-friendly, there's still a learning curve for programming, alarms, and troubleshooting. It requires a commitment to understanding the device.
Navigating the Practical Side of Pump Therapy
So, you've explored whether you might be one of the ideal candidates for insulin pump therapy. Now let's review the practical side of daily life with a pump, from choosing a device to mastering daily care and understanding the financial aspects.

Choosing a Pump: Key Considerations
Choosing an insulin pump is like picking a new smartphone; the best one for you fits your life perfectly. Each pump has unique features to consider.
First, you'll decide between tubed vs. tubeless (patch pumps). Tubed pumps connect to your body with a thin tube, often have a larger insulin reservoir, and can be clipped to clothing. Tubeless patch pumps stick directly to your skin and work wirelessly with a controller, offering more freedom for activities like swimming.
Beyond that, consider water resistance, size and weight, CGM compatibility, smart device integration, ease of use, battery life, and the quality of customer service and training provided by the manufacturer.
Safety and Daily Management
Living with an insulin pump quickly becomes a normal part of your routine. It takes some diligence at first, but soon it'll feel second nature.
One crucial step is infusion site rotation. It's important to change where you place your set every 2-3 days to keep skin healthy, ensure proper insulin absorption, and prevent lumps. You'll also need to change your sets every 2-3 days, including the cannula and reservoir, to prevent infections and ensure the insulin is fresh.
Always have a backup plan. Because pumps use only fast-acting insulin, any interruption in delivery can lead to DKA (Diabetic Ketoacidosis). Keep injectable insulin (both rapid- and long-acting) and supplies on hand. If your pump breaks or your infusion set fails, you need to be able to give yourself insulin right away.
If your blood sugar suddenly shoots up, troubleshooting hyperglycemia usually starts by checking your infusion site for kinks or disconnections. Often, changing the set will fix the problem. If you suspect a pump issue, giving yourself a correction dose via injection is the quickest way to bring your blood sugar down.
Even with a CGM, frequent blood glucose monitoring is still essential. You should check your blood glucose at least four times a day to confirm CGM readings and ensure your pump is working correctly. For more detailed guidance, check out our resource on Living with an Insulin Pump.
Understanding the Costs
The financial side is a big consideration for many candidates for insulin pump therapy. The initial pump cost can be several thousand dollars. Most insurance companies cover this durable medical equipment (DME), but typically only for a new pump every four years.
Beyond the pump, there are ongoing supplies you'll need regularly, including infusion sets, reservoirs, and test strips. These monthly costs can add up, with total yearly costs ranging from $4,500 to $7,200.
When it comes to insurance coverage, most insurers cover insulin pumps and supplies, but they often have specific requirements for approval. Your out-of-pocket expenses will depend on your specific plan's deductible and co-pays.
Be prepared for potential deductibles and out-of-pocket expenses. At ProMed DME, we understand this can be tricky. We work with most insurance plans to help minimize your costs and guide you through coverage complexities. Many manufacturers also offer financial assistance programs. You can find More info about pump benefit programs which might be helpful.
Frequently Asked Questions about Insulin Pump Candidacy
When considering insulin pump therapy, many people have the same questions. Choosing to become one of the candidates for insulin pump therapy is a big decision that affects your daily life. Let's address the most common concerns.
Can I ever take a break from my insulin pump?
Yes, you absolutely can take breaks from your pump! This flexibility is a key benefit of pump therapy. Many people take "pump holidays" for vacations, to give infusion sites time to heal, or simply for convenience.
The key is working with your diabetes care team to make these transitions safely. They'll help you figure out the right injection schedule and insulin doses to keep your blood sugars stable while you're off the pump. It's about choosing what works best for your life at any given moment.
Are insulin pumps suitable for children?
Absolutely! Insulin pumps can be wonderful tools for children with diabetes, with many FDA-approved for kids as young as two years old. For children, the precise dosing capability is especially important, and the flexibility to adjust for meals and playtime is a huge benefit.
However, success really depends on the family's commitment. Parents and caregivers need to be ready to learn the technology, manage blood sugar checks, master carbohydrate counting, and handle troubleshooting. It's a team effort that can be life-changing for the child and the whole family.
Does an insulin pump mean I don't have to check my blood sugar anymore?
This is a common question, but the answer is no. Regular blood sugar monitoring remains absolutely essential, even with the most advanced pump and CGM combination.
Your pump and CGM are smart tools, but you're still the captain of your diabetes management team. You need fingerstick checks to confirm CGM readings before treating highs or lows, especially if the reading doesn't match how you feel. A fingerstick also helps you troubleshoot unexpected high blood sugar to determine if it's a pump problem.
The pump makes insulin delivery more convenient and precise, but it doesn't eliminate the need for you to stay actively involved. Most insurance companies require at least four blood sugar checks per day before approving pump therapy, and that requirement continues once you start.
Conclusión
Deciding if you're one of the ideal candidates for insulin pump therapy is a personal journey. We've covered what these amazing devices are, how they work, who stands to gain the most, and the practicalities of living with this advanced technology.
Choosing a pump is your decision. It requires careful thought, honest self-assessment, and close teamwork with your diabetes care team. While pumps offer incredible precision, amazing flexibility, and the chance for better blood sugar control and an improved quality of life, they also ask for your diligence, a willingness to learn, and a real commitment to safety. It's all about finding the right balance for you.
At ProMed DME, we truly believe in empowering you through technology. We know managing diabetes can feel like a lot to handle, but please know, you're not alone! We're here to support you every single step of the way. Our promise to you includes exceptional customer service, meaning we offer free shipping on your supplies, have a dedicated nurse on staff ready to answer your questions, and we work with most insurance plans to help minimize your out-of-pocket expenses. We're much more than just a supplier; we're your dedicated partner in making your diabetes management smoother and more effective.
Ready to explore further or simply want to learn more about how we can help? Learn more about managing your diabetes with our comprehensive resources.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.




