Beyond the Basics: A Deep Dive into Medicaid's Covered Medical Items

Why Understanding Medicaid Covered Medical Supplies Matters
Medicaid covered medical supplies include a wide range of essential items, from diabetes testing equipment and catheters to wound care dressings and mobility aids. Understanding what your plan covers can save you money and reduce the hassle of obtaining these necessities.
Medicaid Typically Covers:
- Durable Medical Equipment (DME): Wheelchairs, hospital beds, walkers, CPAP machines
- Diabetic Supplies: Glucose monitors, test strips, lancets, insulin syringes
- Incontinence & Urological: Adult diapers, protective underwear, catheters, drainage bags
- Wound Care & Ostomy: Bandages, gauze, specialty dressings, ostomy pouches
- Respiratory Equipment: Nebulizers, oxygen equipment, breathing aids
To Obtain Supplies:
- Get a prescription from your doctor.
- Verify if prior authorization is needed.
- Use a Medicaid-enrolled supplier.
- Supplies are typically shipped to your home with a $0 copay.
Federal regulations require all state Medicaid programs to cover "medical supplies, equipment, and appliances" for home use, but the specifics vary significantly by state. Many people don't realize that Medicaid will pay for items they're currently buying out-of-pocket. The key is knowing what qualifies as "medically necessary" and how to steer the approval process. Unlike Medicare, which requires a 20% coinsurance, Medicaid typically covers supplies at no cost to you.
The challenge is that every state runs its program differently. Some supplies require prior authorization, others have quantity limits, and rules can change depending on your plan. This guide breaks down what medical supplies Medicaid covers, how the approval process works, and the steps to get supplies delivered to your door without unexpected bills.

What Are Durable Medical Equipment (DME) and Medical Supplies?
When navigating Medicaid covered medical supplies, you'll encounter two main categories: Durable Medical Equipment (DME) and consumable medical supplies. Understanding the difference is key to knowing what you can get.

Durable Medical Equipment (DME) refers to reusable items built to last, such as wheelchairs, hospital beds, walkers, and CPAP machines. To qualify as DME, an item must serve a medical purpose, be appropriate for home use, and not be useful to someone without an illness or injury.
Consumable medical supplies are disposable items that need regular replacement. This includes catheters, bandages, ostomy pouches, and glucose test strips. These supplies are typically reordered monthly.
Federal regulations require all state Medicaid programs to cover both DME and medical supplies for home use when they are medically necessary. Both categories require a Certificate of Medical Necessity (CMN) from your healthcare provider, which is an official statement that you need these items to manage your health. For more background, the Medicare Durable Medical Equipment (DME) coverage page provides helpful information that often applies to Medicaid as well.
The "Medically Necessary" Rule
The golden rule for Medicaid covered medical supplies is that an item must be medically necessary. This standard ensures the program's resources are used effectively.
To meet this requirement, a physician, nurse practitioner, clinical nurse specialist, or physician assistant must prescribe the item. They must document that the supply or equipment is essential for treating an illness or injury or preventing a condition from worsening. The item must serve a medical purpose—not just provide comfort or convenience. For example, a hospital bed is medically necessary if you cannot safely use a regular bed, but a premium wheelchair might not be if a standard model works just as well.
Medicaid also follows the least costly alternative principle. If two items can effectively treat your condition, Medicaid will cover the less expensive option. This isn't about denying quality care but using resources wisely. When supplies are truly medically necessary, Medicaid coverage is often more comprehensive than other insurance, with little to no out-of-pocket cost.
Common Categories of Medicaid Covered Medical Supplies
The list of Medicaid covered medical supplies is more extensive than many people realize. While specifics vary by state, this section breaks down the most frequently covered items.
Incontinence and Urological Supplies
Medicaid recognizes that incontinence and urological supplies are medical necessities. Coverage is typically available for anyone aged three and older with incontinence due to a disease, illness, or injury. Covered items often include:
- Adult diapers and protective underwear
- Bladder control pads
- Intermittent catheters and catheter insertion kits
- Drainage bags
These items are vital for maintaining health, dignity, and quality of life.
Wound Care and Ostomy Supplies
Managing a wound or living with an ostomy requires specialized products, most of which fall under Medicaid covered medical supplies. For wound care, coverage typically includes gauze, bandages, medical tape, and specialty dressings like hydrocolloid or foam dressings when medically necessary.
For those with an ostomy, Medicaid generally covers ostomy bags (one-piece and two-piece), skin barriers, and prep wipes to protect the skin around the stoma. These supplies are essential for the approximately one in 500 Americans living with an ostomy.
Diabetic and Respiratory Supplies
For daily health management, certain supplies are essential. For diabetes, Medicaid typically covers:
- Blood glucose monitors, test strips, and lancets
- Insulin syringes and pen needles
Some states, like Florida, are shifting diabetic supplies from the DME benefit to the pharmacy benefit, which changes how you get them but not that they are covered.
For respiratory conditions, coverage is widely available for nebulizers and oxygen equipment. For sleep apnea, CPAP and BiPAP machines and their associated supplies (masks, tubing, filters) are also frequently covered.
Mobility and Home Safety Equipment
Medicaid helps support mobility and home safety by covering a range of equipment. This includes:
- Canes, crutches, and walkers for foundational support.
- Manual and power wheelchairs when a physician deems them medically necessary.
- Hospital beds and patient lifts for more intensive support at home.
- Bedside commodes for safety and convenience.
In most states, all Medicaid beneficiaries are eligible for this equipment, reflecting the program's commitment to helping people stay safe and independent at home.
The Process: How to Get Your Medical Supplies Through Medicaid
Getting your Medicaid covered medical supplies involves a straightforward process: getting a prescription, clearing any administrative problems, and finding the right supplier.

Step 1: Obtain a Prescription from Your Doctor
Everything starts with a prescription from a physician, nurse practitioner, clinical nurse specialist, or physician assistant. This document proves the items are medically necessary for your health condition. Your provider must be thorough in documenting your diagnostic and clinical condition for a smooth approval process. Your prescriber must review your need for medical supplies annually to ensure they are still appropriate.
Step 2: Steer Prior Authorization and Quantity Limits
Your doctor's office or medical supply company will typically handle this paperwork, but it's helpful to know the terms.
- Prior Authorization (PA): This is a pre-approval step where your Medicaid plan reviews the request before covering your supplies. It doesn't mean an item isn't covered, just that more information is needed.
- Quantity Limits: These common restrictions limit how much of a supply you can receive in a given timeframe (e.g., per month). If you need more, your provider must submit additional justification.
- Copayments: While many Medicaid covered medical supplies have a $0 copay, it's always wise to check with your specific plan about potential out-of-pocket costs.
Step 3: Choose a Medicaid-Enrolled Supplier
You must use a DME supplier that is enrolled in and accepts your specific state Medicaid plan. These "in-network providers" are the only ones Medicaid will pay for services.
At ProMed DME, we streamline this process. We work with most insurance plans, including Medicaid, and our team handles the complexities for you. We start by verifying your insurance to confirm what's covered. Then, we manage all the paperwork, coordinating with your doctor to get prescriptions and prior authorizations. Once approved, we arrange for free shipping of your supplies directly to your home, anywhere in the United States. Our dedicated nurse on staff can also answer any questions you have.
While some pharmacies are enrolled as DME suppliers, a specialized company like ProMed DME offers a wider range of products and expertise in navigating complex Medicaid rules.
State Variations and Managed Care Plans
Understanding Medicaid covered medical supplies requires knowing that Medicaid is not a single national program. It's a federal-state partnership, which leads to significant variations in coverage depending on where you live.
Why Coverage Differs from State to State
While federal guidelines mandate coverage for medical supplies, state administration gives each state freedom to define which items are covered, reimbursement rates, and approval processes. A supply automatically covered in one state might require prior authorization or have different quantity limits in another.
For example, Florida shifted diabetic supplies to its pharmacy benefit, while Michigan allows pharmacies to dispense certain respiratory supplies without prior authorization. States also have flexibility with optional benefits, allowing them to expand or limit coverage for certain items based on budgets and priorities. Always check with your specific state's Medicaid program. For a national overview, the Kaiser Family Foundation offers a helpful resource at Medicaid Benefits: Medical Equipment and Supplies.
Fee-for-Service vs. Medicaid Managed Care
How you access Medicaid covered medical supplies also depends on your plan's structure. There are two main models:
- Fee-for-Service Medicaid: The state pays suppliers directly for each item. This model offers more freedom to choose any provider who accepts Medicaid.
- Medicaid Managed Care: Over two-thirds of beneficiaries are in Managed Care Organizations (MCOs), which are private insurance companies that contract with the state. If you're in an MCO, you must use suppliers within that plan's network. MCOs may have their own rules, such as additional prior authorization requirements or a limited list of suppliers.
At ProMed DME, we are experienced in navigating these complexities. We accept most insurance plans, including various Medicaid programs and MCOs. We handle the verification process to confirm your coverage and follow your specific plan's rules, whether it's traditional Medicaid or an MCO. Always contact your plan administrator for details on in-network suppliers and authorization processes.
Medicaid vs. Medicare: Understanding the Key Differences
While both are government health programs, Medicaid and Medicare have key differences regarding Medicaid covered medical supplies. Understanding them can save you money and set clear expectations.
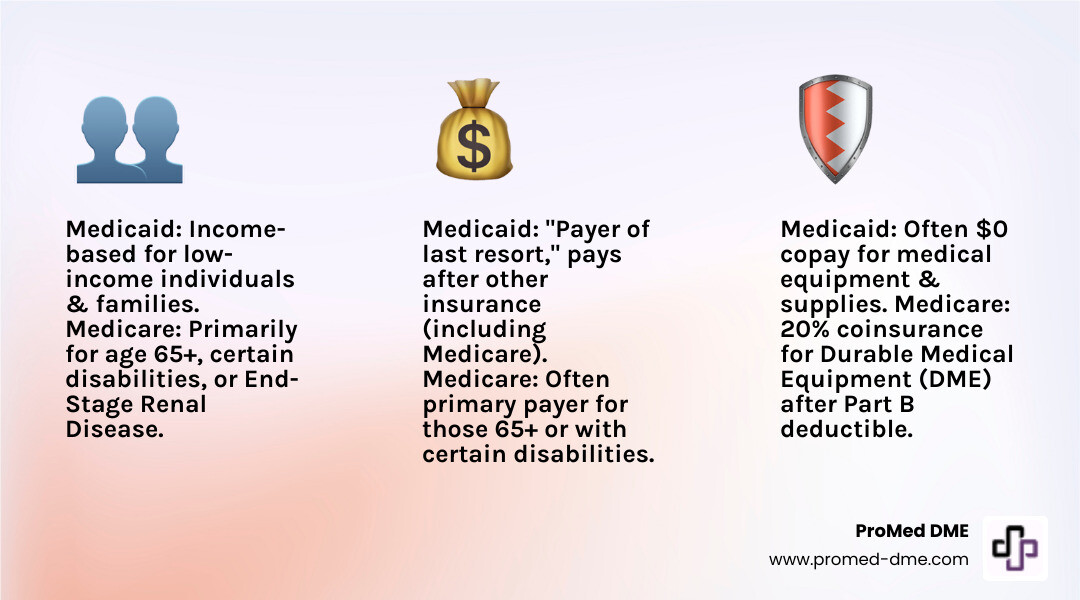
Eligibility: Medicaid is income-based for low-income individuals and families. Medicare is primarily for people aged 65 or older and younger individuals with certain disabilities.
Patient Costs: Medicaid often covers supplies with a $0 copay. With Medicare Part B, after meeting your deductible, you are responsible for 20% of the cost for most durable medical equipment.
Primary Payer: Medicare is typically the primary payer. Medicaid is the "payer of last resort," meaning it pays only after other insurance, including Medicare, has paid its share.
Dual-Eligibility: It's possible to qualify for both programs. In this case, Medicare pays first, and Medicaid may cover the remaining costs, such as the 20% coinsurance, often leaving you with no out-of-pocket expense. For example, if you need a hospital bed, Medicare would cover 80% after your deductible, and Medicaid could cover the remaining 20%.
At ProMed DME, we work with both Medicare and Medicaid plans. We verify your coverage and handle billing coordination to ensure you receive your maximum benefits, whether you're on one program or both.
Frequently Asked Questions about Medicaid Medical Supplies
Here are answers to common questions about navigating Medicaid covered medical supplies.
What items are generally not covered by Medicaid?
Medicaid is designed to cover items that are medically necessary, not everyday household goods or items for convenience. Items that are generally not covered include:
- Common household items: Adhesive tape, rubbing alcohol, cotton swabs, tissue wipes.
- Cosmetics and common remedies: Non-prescription lotions, talc, hydrogen peroxide.
- Items for convenience: A standard recliner for general comfort (as opposed to a prescribed hospital bed).
- Regular food products: Shakes, bars, and regular infant formula (unless it's a prescribed medical formula).
An item must serve a primary medical purpose and be prescribed to qualify. When in doubt, check with your Medicaid plan.
Does Medicaid cover breast pumps?
Yes, Medicaid typically covers breast pumps as a preventive service for new mothers, as they are recognized as medically necessary equipment. You will need a prescription from your healthcare provider. Depending on your state, this may include hospital-grade pumps covered under your medical benefit.
Can I get my supplies from any pharmacy or store?
No. You must use a medical supply company or DME provider that is enrolled in and accepts your specific state Medicaid plan. These are often called "participating providers" or "in-network suppliers." Only enrolled providers can bill Medicaid for your supplies. If you use a non-enrolled provider, you will likely have to pay out-of-pocket.
While some pharmacies are enrolled as DME suppliers, you must confirm this with your plan first. Working with a specialized company like ProMed DME simplifies this. We are enrolled with most insurance plans, including Medicaid programs nationwide. We handle all verification and billing, ensuring your claim is approved. We ship high-quality supplies with free shipping directly to your door, anywhere in the United States, and have a dedicated nurse on staff to answer your questions.
Conclusión
Navigating Medicaid covered medical supplies can be complex, but it doesn't have to be overwhelming. The key takeaway is that Medicaid provides crucial coverage for medically necessary supplies—from catheters and diabetic test strips to wound care and mobility aids—that help you manage your health and maintain independence.
The secret to success is to start with a prescription from your doctor, which documents your medical need. From there, you must work with a Medicaid-enrolled supplier and steer any prior authorization or quantity limit rules.
This is where partnering with the right supplier makes all the difference. At ProMed DME, we make this process easy. We handle insurance verification, tackle the paperwork, coordinate with your doctor, and ship your supplies directly to your door, usually at no cost to you. We work with most insurance plans, including Medicaid programs in all fifty states, and have a dedicated nurse on staff to answer your questions.
Dealing with a chronic condition is hard enough without insurance headaches. If you're ready to simplify your medical supply experience with a team that cares, we're here to help. Explore your medical supply options today and find how much easier managing your health can be with the right partner.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.


