Stay Sweet, Stay Covered—Medicare's Best Glucometers

Why Finding the Right Medicare-Approved Glucometer Matters
Medicare approved glucometers are essential tools for managing diabetes, and understanding what's covered can save you hundreds of dollars each year. Medicare Part B covers blood glucose monitors as durable medical equipment (DME) when prescribed by your doctor for home use.
Quick Answer: What glucometers does Medicare cover?
- Traditional fingerstick monitors - Standard blood glucose meters that use test strips
- Continuous Glucose Monitors (CGMs) - FDA-approved devices from Abbott, Dexcom, Ascensia, and Medtronic
- Implantable CGMs - For patients with frequent low blood sugar episodes
- Related supplies - Test strips, lancets, control solutions, and batteries
Your costs: After meeting your Part B deductible ($257 in 2025), you pay 20% of the Medicare-approved amount.
Managing diabetes effectively requires regular blood sugar monitoring. For millions of people across the globe suffering from diabetes, maintaining constant awareness of their blood sugar levels is a necessary, albeit often challenging, routine. The good news? Medicare covers the tools you need to stay healthy.
Whether you're newly diagnosed or looking to upgrade your current meter, understanding which devices Medicare approves - and how much you'll pay - helps you make the best choice for your health and budget.
The key is working with Medicare-enrolled suppliers who accept assignment. This ensures you only pay your deductible and 20% coinsurance, avoiding surprise bills that can cost hundreds more.
Medicare approved glucometers terms at a glance:
- medicare approved durable medical equipment
- does medicare cover durable medical supplies
- medical supplies medicare covers
Understanding Medicare Coverage for Blood Glucose Monitors
This section explains the fundamentals of how Medicare covers the devices and supplies you need to manage your diabetes effectively.
What Types of Monitors Does Medicare Cover?
The good news is that Medicare approved glucometers come in two main varieties, and Medicare Part B covers both as durable medical equipment (DME). Think of DME as equipment built to last and designed for repeated use in your home.
Traditional fingerstick monitors are the workhorses of diabetes management. These familiar devices require a small drop of blood from your finger, which you place on a test strip for an instant glucose reading. They're reliable, straightforward, and perfect for spot-checking your levels throughout the day. Medicare covers these monitors along with all the supplies you need to keep them running - test strips, lancets, and even the batteries.
Continuous Glucose Monitors (CGMs) are the high-tech option that's becoming increasingly popular. Instead of finger pricks, these systems use a tiny sensor placed under your skin to track your glucose levels around the clock. The sensor talks to a transmitter, which sends your readings to a receiver or smartphone app. What makes CGMs special is their ability to alert you when your blood sugar is heading too high or too low - sometimes before you even feel symptoms.
Medicare covers FDA-approved CGMs from trusted manufacturers, giving you access to some of the most advanced diabetes technology available. These devices can be life-changing for people who struggle with unpredictable blood sugar swings or frequent low glucose episodes.
Both types of monitors serve the same goal: helping you and your doctor understand your glucose patterns so you can make informed decisions about your care. For more detailed information about these monitoring options, check out The two main types of blood glucose monitors.
What are the eligibility requirements for a Medicare approved glucometer?
Getting your Medicare approved glucometers covered is refreshingly straightforward. Medicare wants to make sure the equipment is truly necessary for your health, but the requirements are reasonable and easy to meet.
First, you'll need a confirmed diabetes diagnosis from your doctor. This might seem obvious, but it's the foundation of your coverage - Medicare needs to know you have a medical condition that requires blood glucose monitoring.
Next comes your doctor's prescription. This isn't just any prescription - it needs to spell out exactly why you need the glucometer and how often you'll be using it. Think of your doctor as your advocate here, officially stating that this equipment is essential for managing your health.
Home use is another key requirement. Medicare covers these devices as DME specifically for managing your diabetes at home, not in clinical settings. This makes sense - you're the one living with diabetes 24/7, so you need the tools to monitor it wherever you are.
Finally, either you or a caregiver must be able to learn how to use the device properly. Medicare wants to ensure you'll get accurate readings and can effectively manage your condition. If you need help, that's perfectly fine - a trained family member or caregiver can step in to assist you.
These requirements ensure that the glucometer is "reasonable and necessary" for your diabetes care. You can find the complete details in Medicare's criteria for home blood glucose monitors.
What diabetic supplies besides glucometers does Medicare cover?
Here's where Medicare really shines - it's not just about the Medicare approved glucometers themselves. Medicare Part B understands that effective diabetes management requires a whole toolkit of supplies, and they've got you covered on most of what you'll need.
Blood sugar test strips are your most frequent expense with traditional monitors. Medicare typically covers up to 300 test strips every three months if you use insulin, or 100 strips if you manage diabetes without insulin. If your doctor determines you need more frequent testing for medical reasons, they can request additional strips.
Lancets and lancing devices go hand-in-hand with test strips. These tiny needles and the spring-loaded devices that hold them make getting blood samples quick and relatively painless. Medicare covers these essential tools as part of your monitoring supplies.
Control solution might sound technical, but it's simply a liquid used to check that your glucometer and test strips are working accurately. It's like a quality check for your equipment, and Medicare covers it because accurate readings are crucial for your health.
Even the batteries that power your glucometer are covered. Medicare recognizes that a dead battery shouldn't stand between you and monitoring your blood sugar.
For people using insulin pumps, Medicare Part B covers these external devices as DME, along with the insulin used in them when certain medical conditions are met. This can be a significant cost savings for people who rely on pump therapy.
Syringes, needles, alcohol swabs, and gauze for insulin injections are typically covered under Medicare Part D prescription drug plans, along with inhaled insulin devices. It's worth noting that Part B handles testing supplies while Part D covers most injection supplies and medications.
For a complete breakdown of what's covered, refer to Supplies covered by Medicare Part B.
What documentation is needed from your doctor?
Your doctor is your key ally in getting your Medicare approved glucometers covered, and the documentation they provide makes all the difference between smooth approval and frustrating delays.
A detailed written prescription is your starting point, but this needs to be much more comprehensive than a typical prescription. Your doctor can't just jot down "glucometer" and call it done.
Medical necessity must be clearly explained. Your doctor needs to document exactly why you need this specific equipment to manage your diabetes effectively. This connects your individual health needs to the equipment you're requesting.
Diagnosis confirmation ties everything together by officially stating your diabetes diagnosis in your medical record. This satisfies Medicare's requirement that you have a qualifying condition.
Testing frequency instructions are crucial because they determine how many supplies you'll receive. If your doctor prescribes testing four times daily, Medicare will approve more test strips than if you only need to test once a day. This frequency should match your actual medical needs and treatment plan.
Quantity of supplies needed flows directly from your testing frequency. Your doctor will calculate how many test strips, lancets, and other supplies you'll need over a three-month period based on your prescribed testing schedule.
This thorough documentation ensures Medicare understands your specific situation and can process your claims without delays. Working closely with your healthcare provider to get all the paperwork right from the start saves time and prevents headaches later.
Navigating Costs and Specific Medicare Approved Glucometers
Knowing what Medicare covers is the first step. Next is understanding the costs involved and which specific types of devices are approved.
What is the cost of glucometers with Medicare Part B?
Let's talk money – because understanding your costs upfront helps you budget for your diabetes supplies without any surprises. While Medicare approved glucometers are covered under Part B, you'll still have some out-of-pocket expenses.
Think of it this way: Medicare is your partner in paying for these essential devices, but you're still responsible for your share. First, you'll need to meet your annual Part B deductible, which is $257 in 2025. This means you'll pay the first $257 out of your own pocket for all your Medicare Part B services combined – not just your glucometer.
Once you've met that deductible, Medicare picks up 80% of the Medicare-approved amount, and you pay the remaining 20% as coinsurance. So if your glucometer supplies have a Medicare-approved amount of $100, you'd pay $20 while Medicare covers the other $80.
Here's where it gets important: always work with suppliers who accept assignment. When a supplier accepts assignment, they agree to take the Medicare-approved amount as full payment. This protects you from surprise bills that could be hundreds of dollars more than expected.
If a supplier doesn't accept assignment? Well, they can charge you whatever they want above the Medicare amount, and you could end up paying significantly more. That's definitely not what you want when you're managing a chronic condition like diabetes.
For detailed information about Medicare costs, check out Understanding Medicare costs.
Are specific brands of Medicare approved glucometers covered?
You might be wondering if your favorite brand of glucometer is covered by Medicare. The good news is that Medicare focuses on covering FDA-approved devices that meet their medical necessity requirements, rather than excluding specific brands.

For traditional fingerstick monitors, most major brands that are FDA-approved will be covered. The key is making sure your supplies come from a Medicare-enrolled supplier who stocks the brand you prefer.
When it comes to Continuous Glucose Monitors (CGMs), Medicare covers several well-known brands that have received FDA approval. These include Abbott's FreeStyle Libre systems, Dexcom's G6 and G7 systems, Ascensia devices, and Medtronic's Guardian systems. These aren't just any old devices – they're sophisticated pieces of technology that can dramatically improve how you manage your diabetes.
The beauty of CGMs is that they give you a complete picture of your glucose levels throughout the day and night, rather than just a snapshot when you do a fingerstick test. They can even alert you when your levels are getting too high or too low, which can be a real game-changer for your health and peace of mind.
Your doctor will help determine which type of device is best for your specific situation, and they'll make sure to prescribe something that Medicare covers. For more details on FDA-approved CGM brands, you can explore FDA-approved CGM brands covered by Medicare.
What are the criteria for Medicare to cover implantable continuous glucose monitors (I-CGMs)?
Implantable Continuous Glucose Monitors represent the cutting edge of diabetes technology. These devices are inserted under your skin and can monitor your glucose levels for months at a time. Pretty amazing, right? But because they're more intensive than regular glucometers, Medicare has stricter requirements for coverage.
Medicare typically covers I-CGMs when you meet specific clinical criteria that show you really need this advanced level of monitoring. The most important requirement is that you must be using insulin to manage your diabetes. These devices are designed for people whose diabetes requires precise, ongoing management.
You'll also need to have a history of problematic hypoglycemia – meaning you've had multiple episodes of dangerously low blood sugar despite following your treatment plan. This shows that standard monitoring methods aren't giving you the control you need to stay safe.
Another key factor is impaired hypoglycemic awareness. Some people with diabetes lose the ability to feel when their blood sugar is dropping too low, which can be extremely dangerous. An I-CGM can provide crucial alerts that help prevent serious complications.
Your doctor will need to provide detailed documentation explaining why you meet these criteria and why an implantable device is medically necessary for your specific situation. This isn't just paperwork – it's about making sure you get the right level of care for your unique needs.
These requirements might seem strict, but they ensure that I-CGMs go to patients who will benefit most from this advanced technology. Your healthcare team will be your best guide in determining if you qualify. You can find the official criteria at Medicare criteria for implantable CGMs.
CGMs and Medicare Advantage Plans
Continuous Glucose Monitors (CGMs) are a modern solution for diabetes management. Here's how they are covered by Original Medicare and Medicare Advantage plans.
Does Medicare cover continuous glucose monitors (CGMs)?
Yes, Medicare Part B absolutely covers Continuous Glucose Monitors! These sophisticated devices fall under durable medical equipment (DME) coverage, and they're considered therapeutic CGMs because they help you make real-time treatment decisions about your diabetes care.
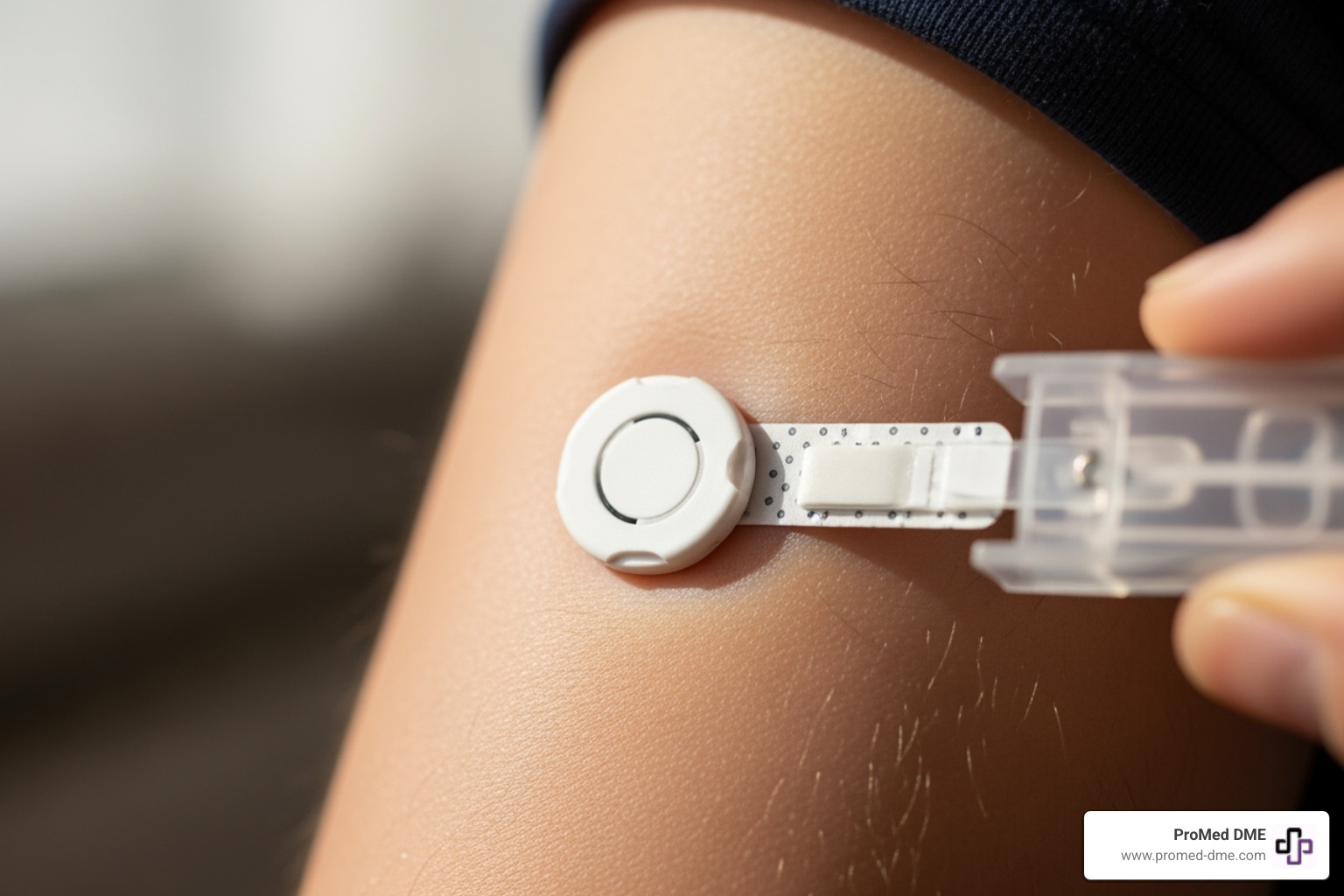
Think of CGMs as your personal glucose assistant that never sleeps. Unlike traditional Medicare approved glucometers that give you a snapshot when you test, CGMs provide continuous monitoring through sensors, transmitters, and receivers that work together 24/7.
To qualify for CGM coverage under Medicare, you'll need to meet specific medical criteria. A diabetes diagnosis is the starting point, but Medicare also requires that you're either taking insulin or have a history of problematic hypoglycemia despite treatment. This makes sense - CGMs are particularly valuable for people who need close monitoring because their blood sugar can be unpredictable.
Your doctor must provide a detailed prescription that includes how often you should check your readings and any specific monitoring instructions. You'll also need to be trained on proper use - either you or a caregiver must understand how to operate the device correctly and interpret the results.
Routine doctor visits are another requirement. Medicare wants to ensure you're getting proper medical oversight, whether through in-person appointments or Medicare-approved telehealth visits. This ongoing relationship with your healthcare provider helps ensure the CGM is truly improving your health outcomes.
The beauty of CGMs lies in their real-time alerts and trend information. They can warn you when your blood sugar is heading too high or too low, often before you'd even think to test with a traditional meter. This early warning system can prevent dangerous situations and give you much better control over your daily diabetes management.
How does Medicare Advantage (Part C) coverage differ from Original Medicare?
Here's where things get a bit more nuanced. Medicare Advantage plans must cover everything that Original Medicare covers - that's the law. So if Original Medicare covers your Medicare approved glucometers or CGMs, your Medicare Advantage plan has to cover them too.

But the devil is in the details, as they say. While the basic coverage is the same, how you access that coverage and what you pay can be quite different.
Your costs might change significantly. Instead of Original Medicare's standard 20% coinsurance after you meet your deductible, Medicare Advantage plans often use different copayment structures. You might pay a flat $20 copay for diabetes supplies, or perhaps a different coinsurance percentage. Some plans have separate deductibles just for medical equipment.
Network restrictions are probably the biggest difference you'll encounter. Medicare Advantage plans typically require you to use in-network suppliers to get the best coverage. While Original Medicare lets you visit any Medicare-enrolled supplier nationwide, your Medicare Advantage plan might have a specific list of preferred DME suppliers. Using an out-of-network supplier could mean higher costs or even no coverage at all.
Plan-specific rules can also affect your experience. Some Medicare Advantage plans require prior authorization for CGMs, even though Original Medicare doesn't. Others might have preferred brands or models listed in their formularies, potentially steering you toward certain devices.
The key is understanding your specific plan's rules before you need supplies. Each Medicare Advantage plan is different, so what works for your neighbor might not apply to your coverage. We always recommend checking your plan's Evidence of Coverage document or calling them directly to understand exactly how they handle diabetes supplies.
To compare different plans and their specific coverage details, the Medicare plan finder tool can help you see how various options might affect your out-of-pocket costs for the diabetes supplies you need.
How to Get Your Medicare-Covered Diabetes Supplies
Follow these steps to ensure you get the right supplies with minimal out-of-pocket costs.
Where can beneficiaries obtain Medicare-covered diabetic supplies?
Finding the right place to get your Medicare approved glucometers and supplies doesn't have to be complicated. The secret is working with suppliers who know Medicare inside and out and can help you avoid those dreaded surprise bills.
Your best options are Medicare-enrolled DME suppliers - these are the specialists who live and breathe durable medical equipment. They understand all the Medicare rules and requirements, which means fewer headaches for you. Many of these suppliers have been working with Medicare patients for years and can guide you through the process smoothly.
Participating pharmacies are another great choice, especially for ongoing supplies like test strips and lancets. Your local pharmacy might already be enrolled with Medicare, making it super convenient to pick up refills while you're getting other prescriptions.
Here's the golden rule: always ask if they accept assignment. When a supplier accepts assignment, they agree to Medicare's approved amount as full payment. This means you only pay your deductible and 20% coinsurance - no surprise bills that could cost you hundreds more.
At ProMed DME, we take the guesswork out of this process. We're Medicare-enrolled and work with most insurance plans to keep your costs as low as possible. Based in Stuart, Florida, we ship nationwide and handle all the paperwork so you can focus on managing your health, not wrestling with insurance forms.
What is the step-by-step process?
Getting your Medicare approved glucometers should feel like a well-oiled machine, not a puzzle you're trying to solve. We've broken it down into simple steps that take the stress out of the process.
Step 1: Visit your doctor. This is where everything starts. Your doctor will evaluate your diabetes management needs and determine whether you need a traditional fingerstick monitor or a continuous glucose monitor. They'll also confirm that the device is medically necessary for your specific situation.
Step 2: Get a detailed prescription. Your doctor needs to provide a comprehensive written prescription that includes your diabetes diagnosis, the specific equipment you need, testing frequency, and quantity of supplies required. Think of this as your roadmap - the more detailed it is, the smoother your journey will be.
Step 3: Find a Medicare-enrolled supplier that accepts assignment. This step is crucial for keeping your costs manageable. You can ask your doctor for recommendations or choose a trusted provider. The key is confirming they're Medicare-enrolled and accept assignment before placing your order.
Step 4: Place your order. Once you have your prescription and supplier lined up, it's time to get your supplies. At ProMed DME, we make this step effortless by contacting your doctor directly for the prescription, verifying your insurance coverage, and handling all the paperwork. Plus, we offer free shipping to your door.
Step 5: Set up refills. Managing diabetes is a marathon, not a sprint, so you'll need regular refills of test strips, lancets, and CGM sensors. A good supplier will help you stay ahead of running out by setting up automatic deliveries. Our dedicated nurse is always available to answer questions about your supplies and help ensure you never miss a beat in your diabetes management routine.
Following these steps ensures you get your Medicare approved glucometers and supplies without the usual insurance hassles. We believe managing your health should be straightforward and stress-free.
Conclusión
Managing your diabetes doesn't have to feel overwhelming when you understand your Medicare benefits and have the right support system in place. Throughout this guide, we've walked through everything you need to know about Medicare approved glucometers - from traditional fingerstick meters that have been trusted for decades to the latest continuous glucose monitors that provide real-time insights into your blood sugar patterns.
The key takeaway? Medicare Part B has your back when it comes to diabetes management tools. Whether you need a basic glucose meter for daily testing or an advanced CGM system for round-the-clock monitoring, Medicare covers these essential devices as durable medical equipment. After you meet your annual deductible of $257 in 2025, you'll typically pay just 20% of the Medicare-approved amount when you work with suppliers who accept assignment.
Your doctor plays a crucial role in this process - they're not just prescribing a device, they're creating a roadmap for your diabetes management. Their detailed prescription ensures Medicare understands exactly why you need specific equipment and supplies, from test strips to lancets to CGM sensors.
The most important advice we can share? Choose your supplier wisely. Working with a Medicare-enrolled supplier who accepts assignment protects you from unexpected bills and complicated reimbursement processes. You want a partner who understands the ins and outs of Medicare coverage and can handle the paperwork while you focus on your health.
At ProMed DME, we've built our entire approach around making diabetes supply management as simple as possible. Our dedicated nurse is always available to answer your questions, we handle all the insurance paperwork, and we ship your supplies directly to your door at no extra cost. We know that managing diabetes is a full-time job - let us take care of the supply logistics so you can concentrate on living your best life.
Ready to get started with your Medicare approved glucometers and diabetes supplies? Contact us for your diabetes supply needs and experience the difference that personalized service and genuine care can make in your diabetes management journey.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.



