Don't Get Pricked by Costs: Medicare Coverage for Insulin Syringes
Why Understanding Medicare Coverage for Insulin Syringes Matters
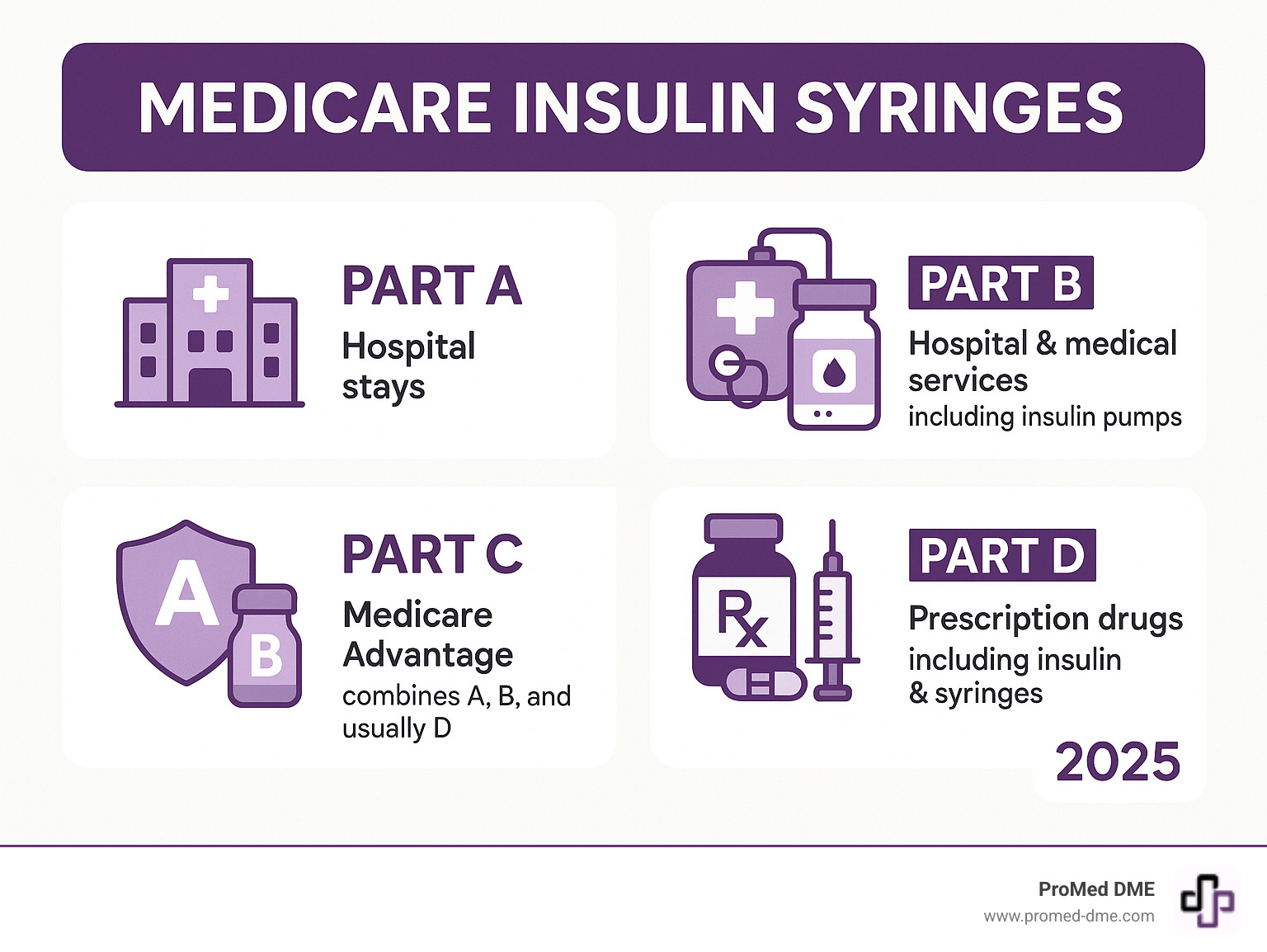
Medicare insulin syringes are covered under Medicare Part D (prescription drug coverage), not Part B, when used for self-injection. Here's what you need to know:
- Part D Coverage: Insulin syringes, needles, alcohol swabs, and gauze are covered when prescribed for insulin injection
- Part B Limitation: Only covers insulin used with durable insulin pumps, not injection supplies
- Cost: Varies by plan - syringes are NOT included in the $35 insulin cap
- Requirements: Valid prescription and in-network pharmacy required
- Plan Check: Coverage depends on your specific Part D plan's formulary
With 8.4 million Americans relying on insulin according to the American Diabetes Association, understanding Medicare coverage is essential for your health and wallet.
The confusion is real. Many people assume that since Part B covers some diabetes supplies like test strips, it would also cover insulin syringes. It doesn't. This common misunderstanding can lead to unexpected costs.
Medicare's coverage rules split diabetes supplies across its different parts. While the $35 monthly insulin cap helps with medication costs, the supplies you need to inject that insulin follow different rules entirely.
Simple guide to Medicare insulin syringes:
The Great Divide: Is It Medicare Part B or Part D for Syringes?
Which part of Medicare covers your Medicare insulin syringes? The answer can be confusing and depends on how you take your insulin. Let's break it down.
Medicare Part B: Coverage for Pumps, Not Syringes
Medicare Part B covers durable medical equipment (DME)—items built to last for medical use at home. When it comes to diabetes care, Part B steps up to cover insulin pumps and the insulin that goes with them.
If you're using an external insulin pump, you're in luck with Part B. It covers the pump itself because it qualifies as DME. Think of it like a medical appliance that delivers insulin throughout the day.
Part B also covers the insulin used specifically with these pumps. So if you're a pump user, your insulin costs fall under Part B coverage rules.

But here's where Part B draws the line: it does not cover injection supplies for people who self-inject insulin. This means no coverage for syringes, needles, alcohol swabs, or any other supplies you need to give yourself insulin shots.
This may seem backward, but it's due to how Medicare categorizes items. Pumps are considered DME, while injection supplies fall into a different category.
Understanding Part D Coverage for Medicare insulin syringes
Now for the good news for people who self-inject insulin: Medicare Part D is where you'll find coverage for insulin syringes and other injection supplies.
Part D plans are prescription drug plans, and they cover much more than just pills. With Part D coverage (either through a standalone plan or a Medicare Advantage plan), you get coverage for self-injected insulin and the medical supplies needed to inject it safely.
This includes your Medicare insulin syringes, needles, alcohol swabs, and gauze. Basically, if you need it to give yourself an insulin injection, Part D likely covers it.
Remember: each Part D plan has its own formulary—the official list of what they cover. While most plans cover insulin syringes, the specific brands or types might vary.
You'll also want to get your supplies from an in-network pharmacy to keep your costs as low as possible. This ensures you're getting the best price your plan has negotiated.
For official details about what Medicare covers for diabetes supplies, check out the Official Medicare guide to diabetes supplies. It's your go-to resource for understanding exactly what's covered.
The bottom line? If you're using an insulin pump, look to Part B. If you're giving yourself insulin shots, Part D is your friend for both the insulin and the supplies.
Navigating Costs and Requirements for Your Supplies
Getting your Medicare insulin syringes without breaking the bank requires understanding the practical details. Let's review what you need to know to keep costs predictable and your supplies flowing.
What are the out-of-pocket costs for Medicare insulin syringes?
Medicare Part D costs for Medicare insulin syringes vary. Your out-of-pocket expenses depend on your plan's coverage phases and how it structures costs.
Most Part D plans start with an annual deductible you'll need to meet before coverage kicks in. After that, you'll typically pay either a copayment (a fixed dollar amount, like $15 for a month's supply) or coinsurance (a percentage of the total cost, such as 25%).
The exact amount also depends on which tier your supplies land on in your plan's formulary. Plans organize drugs and supplies into different tiers—lower tiers mean lower costs for you.
Now, here's something that catches many people off guard: the $35 monthly insulin cap is fantastic news for your insulin costs, but it doesn't extend to your injection supplies. Your Medicare insulin syringes, needles, and alcohol swabs will still be subject to your plan's regular cost-sharing rules. We know it seems a bit backwards, but that's how the coverage works.

Documentation Needed from Your Doctor
To get your Medicare insulin syringes covered, you need the right paperwork. Your doctor's prescription is the key, as it must demonstrate medical necessity to Medicare.
The prescription itself needs to be thorough and specific. Your doctor should clearly state your diabetes diagnosis and spell out exactly what you need, listing Medicare insulin syringes, needles, alcohol swabs, and gauze separately. The quantity and frequency also matter—whether you need 100 syringes per month or a 90-day supply, that detail helps ensure smooth processing.
Once your doctor submits this detailed prescription, the pharmacy or medical supplier will handle the insurance paperwork. A little extra detail upfront can save you a lot of headaches later.
Where to Purchase Medicare-Covered Syringes
Finding the right place to buy your Medicare insulin syringes is key to controlling costs. You have several solid options.
In-network pharmacies are usually your best bet for convenience and predictable copays. Most major pharmacy chains participate in multiple Part D networks.
Mail-order services through your Part D plan can be convenient, often allowing 90-day supplies delivered to your door, sometimes at lower costs.
Medicare-enrolled medical suppliers are another option. At ProMed DME, we work with most insurance plans and understand the ins and outs of Medicare coverage, which can make the whole process smoother for you.
A crucial tip: always confirm that your supplier accepts assignment. This means they agree to accept Medicare's approved amount as full payment. If they don't, they can charge you extra. Don't be shy about asking—any reputable supplier will clarify their Medicare policies upfront.
Insulin vs. Syringes: How Medicare Coverage Differs
It's a common misconception that if Medicare covers your insulin, it also covers all related supplies. Unfortunately, Medicare treats them as separate items with different coverage and pricing rules.
| Coverage Item | Medicare Part | Monthly Cost Cap | Deductible | Coverage Details |
|---|---|---|---|---|
| Insulin for pumps | Part B | $35 per insulin type | Usually no deductible | Covers pump + insulin |
| Injectable insulin | Part D | $35 per insulin type | Varies by plan | Self-injection insulin |
| Insulin syringes | Part D | No cap - varies by plan | Subject to plan deductible | Must check formulary |
| Needles & supplies | Part D | No cap - varies by plan | Subject to plan deductible | Coverage varies by plan |
Insulin Coverage Explained
The good news is that the Inflation Reduction Act caps your insulin costs at $35 per month for each type of insulin you use. This applies whether you're getting a one-month supply or a three-month supply (which would cost no more than $105 total).
This cap is a game-changer. It doesn't matter if you have Extra Help or not—everyone pays the same maximum amount. And if you use an insulin pump covered by Part B, you typically don't have to pay a deductible for your insulin.
Part B covers insulin when it's used with a durable medical equipment insulin pump. The pump and the insulin are both covered under this part of Medicare.
Part D covers insulin that you inject yourself with syringes or pens, plus any inhaled insulin. The same $35 monthly cap applies here too.
This predictable pricing makes it much easier to budget for your diabetes care. For all the details on how this works, check out More on Medicare's insulin coverage.
Syringe and Supply Coverage Explained
The rules for your Medicare insulin syringes and other injection supplies are completely different. They do not fall under the predictable $35 cap.
Part D is your coverage source for syringes, needles, alcohol swabs, and gauze when you're self-injecting insulin. These supplies are considered medical necessities for using your prescription insulin.
But here's the catch: coverage varies significantly by plan. Unlike insulin's standard $35 cap, each Part D plan sets its own rules for covering these supplies. Your neighbor might pay $10 for a month's worth of syringes while you pay $25, simply because you have different plans.
The $35 cap doesn't apply to your injection supplies—only to the insulin itself. This is the most important thing to remember.
Your formulary is everything when it comes to these supplies. This is your plan's official list of what's covered and what you'll pay. Some plans might cover generic syringes with a low copay, while others might require you to meet your deductible first. The only way to know for sure is to check your specific plan's formulary or call them directly.
It's also worth checking if your plan has quantity limits. Understanding these details upfront helps you avoid surprises at the pharmacy counter.
How Medicare Advantage and Other Programs Can Help
When it comes to managing diabetes and getting your Medicare insulin syringes, there are options beyond Original Medicare that might offer better coverage or help stretch your dollars further.
Medicare Advantage (Part C) Plans
Medicare Advantage Plans are an all-in-one package deal. These private insurance plans must cover everything Original Medicare does, and many go above and beyond those basic requirements.
Most Medicare Advantage Plans include prescription drug coverage, which means your Medicare insulin syringes and other supplies would be covered under that integrated benefit. This bundles your health and prescription coverage, often with extras.
The trade-off? These plans typically require you to use doctors, hospitals, and pharmacies within the plan's network to get the best coverage.
Some Medicare Advantage Plans offer Chronic Special Needs Plans (C-SNPs) designed for people with conditions like diabetes. These specialized plans might offer improved benefits like lower copays for diabetic supplies, wellness programs, or care coordination services.
Costs can be different too. Your deductibles, copayments, and coinsurance might vary compared to Original Medicare. Some people find they save money, while others prefer the predictability of Original Medicare.
If you're considering a switch, review the plan's Summary of Benefits and formulary. Make sure your doctors and pharmacy are in-network, and check how they handle your insulin and Medicare insulin syringes.
Finding Financial Assistance
Managing diabetes can be expensive, even with Medicare. If you need help, resources are available to lighten the financial load.
Your doctor might know about patient assistance programs from pharmaceutical companies that can provide free or discounted insulin. Companies like Novo Nordisk, Eli Lilly, and Sanofi have programs to help people who are struggling financially. You can explore these at Find Patient Assistance Programs.
Some states have their own State Pharmaceutical Assistance Programs (SPAPs) that help residents pay for prescriptions. These programs vary by state, so it's worth checking what's available at Check for State Pharmaceutical Assistance Programs.
Don't overlook Medicare Part B's coverage for Diabetes Self-Management Training. You may be eligible for up to 10 hours of outpatient training that can teach you money-saving strategies for managing your diabetes.
Discount programs and coupon sites can also provide real savings. Services like BenefitsCheckUp.org from the National Council on Aging can help you find programs you might not know existed.
No one should have to choose between paying for their medication and other necessities. Don't hesitate to explore your options—you might be surprised at how much help is available.
Frequently Asked Questions about Medicare Insulin Syringes
Medicare can be confusing. Here are answers to the most common questions we hear about Medicare insulin syringes to help you make sense of your coverage.
Does Original Medicare Part B cover insulin syringes for self-injection?
No, Original Medicare Part B does not cover insulin syringes for self-injection. This may seem backward, especially since Part B covers other diabetes supplies like blood glucose test strips, but the rules are different.
The confusion is understandable. Many people think that if Medicare covers doctor visits and some supplies, it should cover daily-use syringes. Unfortunately, that's not how it works.
Medicare Part B will cover insulin, but only when used with an external insulin pump that qualifies as durable medical equipment. Part B covers the "big ticket" medical equipment, but not the day-to-day supplies for self-care.
The official Medicare policy is clear: Medicare insulin syringes used for self-injection don't meet the requirements for Part B coverage under the "incident to a physician's professional service" rule. That rule applies to supplies administered in a doctor's office, not supplies you use at home.
So if you're giving yourself insulin injections, you'll need to look to Medicare Part D for coverage of your syringes, needles, and other supplies.
Are there specific types or brands of insulin syringes that Medicare covers?
Coverage for specific syringe brands isn't universal. It depends entirely on your specific Medicare Part D plan's formulary.
Think of a formulary as your plan's menu of covered drugs and supplies. One plan might cover a wide range of Medicare insulin syringes, while another may only cover certain preferred brands or gauges.
Your plan's formulary will tell you exactly which types and brands are covered, and it might specify details like needle length or syringe capacity. Some plans prefer certain manufacturers because they've negotiated better prices, which can mean lower costs for you.
The best way to find out what's on your plan's "menu" is to check your plan's formulary directly. You can usually find this on your plan's website or by calling the number on your member ID card. Your pharmacist is also a great resource, as they can quickly tell you what your plan covers.
Formularies can change annually, so it's worth double-checking during open enrollment.
Are there limits on how many syringes I can get?
Yes, and this helps keep your costs predictable. Medicare Part D plans typically set quantity limits based on what is medically appropriate for your situation.
These limits are based on your doctor's prescription. For example, if you inject insulin twice a day, your doctor might prescribe 60 syringes for a 30-day supply, and your plan will generally cover that amount.
Most plans work with standard 30-day or 90-day supplies. The exact numbers depend on your prescription and your plan's rules.
If your doctor determines you need more supplies than your plan's standard limit allows, there's a process for that. Your doctor can submit a prior authorization request explaining why you need the additional supplies, perhaps due to a change in your injection schedule.
The key is to maintain communication with your doctor and your Part D plan. Working together, they can usually find a solution that keeps you well-supplied.
Conclusión
Navigating Medicare for diabetes supplies can seem overwhelming, but with the right information, you can confidently manage your healthcare needs and costs.
Here's the bottom line: Medicare insulin syringes and other injection supplies are covered under Medicare Part D, not Part B. This distinction is critical because it affects where you get your supplies, how much you pay, and what documentation you need. While Medicare made insulin more affordable with the $35 monthly cap, the supplies for injection follow different rules and costs.
Your Part D plan's formulary is your best friend in this journey. It's your personalized guide to what's covered, what you'll pay, and any limits that apply. Plans vary significantly, so we encourage you to review your formulary at least once a year during open enrollment and call your plan with any questions.
You also have options beyond Original Medicare. Medicare Advantage plans might offer additional benefits for diabetes management, and various assistance programs exist to help with costs. Whether it's state programs or manufacturer assistance, help is available.
At ProMed DME, we understand that managing diabetes is about more than just medical supplies—it's about maintaining your quality of life. We're here to make the supply side of your care as simple as possible. Based in Stuart, Florida, we ship nationwide and work with most insurance plans to minimize your out-of-pocket costs. Our dedicated nurse is available to answer your questions, and we provide free shipping because accessing the supplies you need shouldn't be a financial burden.
With the knowledge you've gained and a reliable partner for your supplies, you can focus on what really matters: living your best life while effectively managing your diabetes.
Recursos y artículos relacionados
Manténgase informado con las entradas de nuestro blog informativo.
Descubra las ventajas de ProMed
y pruebe nuestros productos
Ofrecemos envío gratuito y un legendario servicio de atención al cliente para garantizar que reciba los
mejores productos de DME para sus necesidades.




